1. What is diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes that affects the eyes. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye.
The damage to the blood vessels can cause them to leak fluid or blood into the retina, which can result in blurred or distorted vision. In some cases, the blood vessels may also close off, leading to the growth of abnormal blood vessels that can cause further damage to the retina and potentially lead to blindness if left untreated.
Diabetic retinopathy is the most common cause of vision loss among people with diabetes, but it can often be prevented or treated with early detection and proper management of blood sugar levels. Regular eye exams are important for people with diabetes to detect any signs of retinopathy early on.
2. What are the symptoms of diabetic retinopathy?
In its early stages, diabetic retinopathy may not cause any noticeable symptoms. However, as the condition progresses, the following symptoms may occur:
- Blurred or distorted vision
- Difficulty seeing at night
- Floaters, or dark spots or strings that appear to float across the field of vision
- Sudden loss of vision in one or both eyes
- Eye pain or pressure
- Reduced color sensitivity
If you have diabetes and experience any of these symptoms, it’s important to see an eye doctor right away. However, it’s important to note that some people with diabetic retinopathy may not experience any symptoms until the condition has progressed to a more advanced stage, which is why regular eye exams are so important for people with diabetes.
3. What causes diabetic retinopathy?
Diabetic retinopathy is caused by damage to the blood vessels in the retina, which can occur as a result of high blood sugar levels over time. The exact mechanism by which high blood sugar damages the blood vessels is not fully understood, but it is thought to involve a number of factors, including
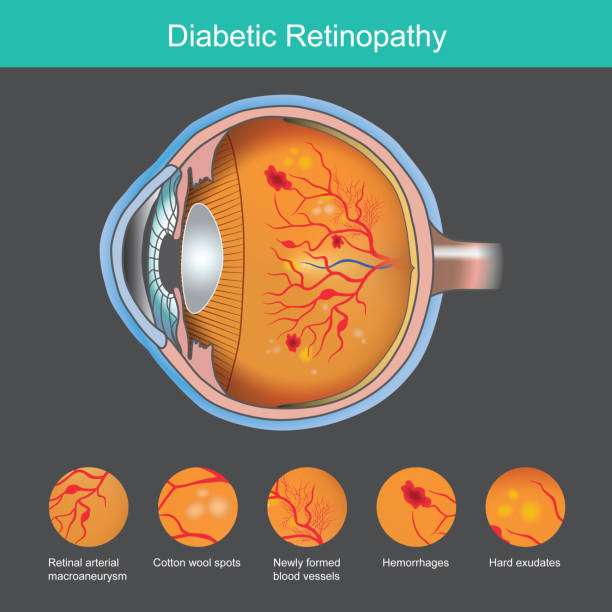
- Damage to the small blood vessels: High blood sugar levels can damage the small blood vessels that supply blood to the retina, leading to leakage of fluid and blood into the retina.
- Changes in the retinal blood vessels: High blood sugar levels can cause the blood vessels in the retina to become narrow, blocked, or leaky. This can lead to the growth of abnormal blood vessels, which can cause further damage to the retina.
- Inflammation: Chronic inflammation caused by high blood sugar levels can contribute to the development of retinopathy.
- Genetics: Some people may be more genetically predisposed to developing retinopathy than others.
- Other medical conditions: High blood pressure and high cholesterol can also contribute to the development and progression of diabetic retinopathy.
It’s important for people with diabetes to manage their blood sugar levels, blood pressure, and cholesterol levels to reduce their risk of developing diabetic retinopathy. Regular eye exams are also important for early detection and treatment of the condition.
4. What are the different types of diabetic retinopathy?
There are two main types of diabetic retinopathy:
- Non-proliferative diabetic retinopathy (NPDR): This is the earlier and more common stage of diabetic retinopathy, where the blood vessels in the retina are damaged, but new blood vessels have not yet started to grow. NPDR can be further classified into mild, moderate, and severe stages, depending on the degree of damage to the blood vessels.
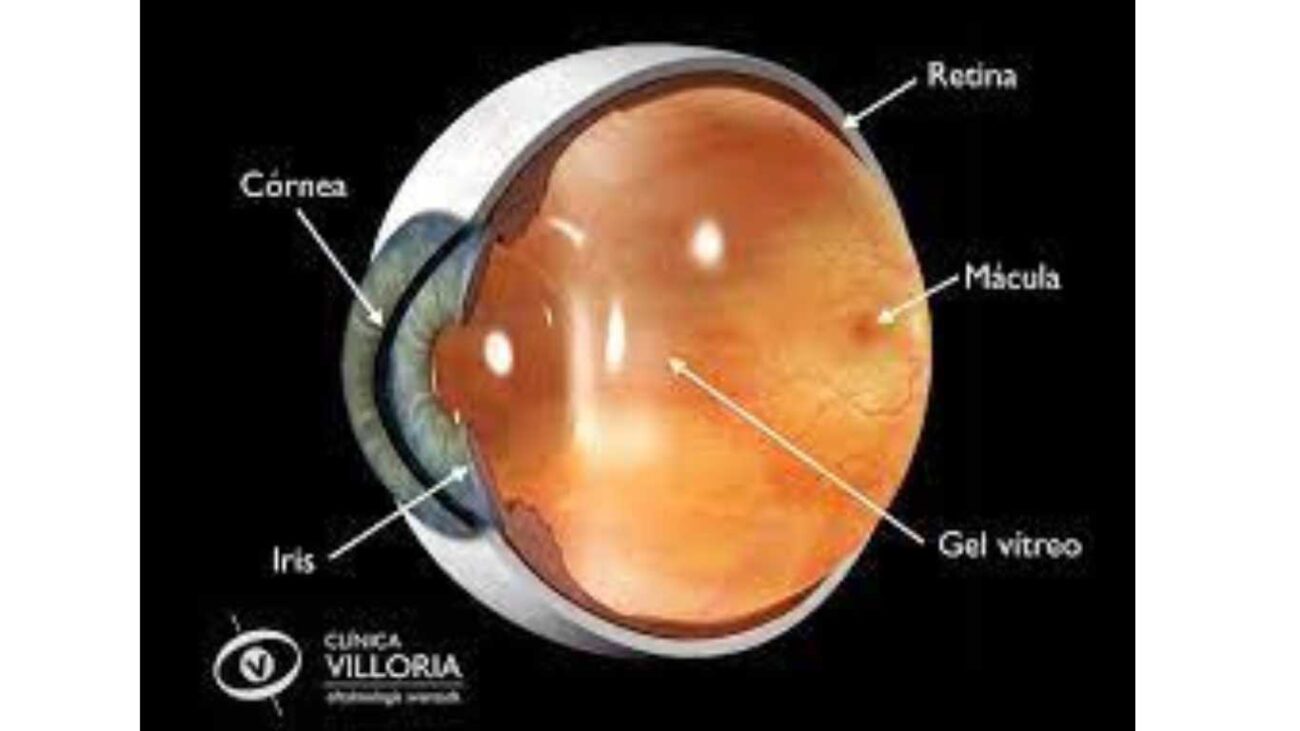
- Proliferative diabetic retinopathy (PDR): This is the more advanced stage of diabetic retinopathy, where new abnormal blood vessels begin to grow in the retina. These new blood vessels are fragile and can leak blood into the vitreous gel, which fills the center of the eye. PDR can cause severe vision loss or blindness if not treated promptly.
Additionally, there are other types of diabetic retinopathy, including
- Diabetic macular edema (DME): This occurs when fluid leaks into the macula, which is the part of the retina responsible for central vision. DME can occur at any stage of diabetic retinopathy and can cause severe vision loss if left untreated.
- Ischemic diabetic retinopathy: This occurs when the blood supply to the retina is reduced, which can lead to the growth of abnormal blood vessels and severe vision loss.
The type and severity of diabetic retinopathy can vary from person to person and can also differ between the two eyes of the same person. Regular eye exams are important for detecting and monitoring any changes in the eyes caused by diabetes.
5. How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed through a comprehensive eye exam that includes the following tests:
- Visual acuity test: This test measures how well you can see at different distances.
- Dilated eye exam: In this exam, the eye doctor will use eye drops to dilate (widen) the pupils and examine the back of the eye, including the retina and optic nerve, for any signs of diabetic retinopathy.
- Tonometry: This test measures the pressure inside the eye and can help detect conditions like glaucoma.
- Optical coherence tomography (OCT): This non-invasive imaging test uses light waves to create detailed images of the retina and can detect any swelling or thickening in the macula caused by diabetic macular edema.
- Fluorescein angiography: This test involves injecting a special dye into a vein in your arm, which travels to the blood vessels in your eyes. Pictures are then taken of your retina as the dye passes through the blood vessels. This test can detect any abnormal blood vessel growth or leakage in the retina.
If diabetic retinopathy is detected, the eye doctor may recommend additional tests or refer you to a specialist for further evaluation and treatment. It’s important for people with diabetes to have regular eye exams, at least once a year, to detect any signs of diabetic retinopathy early on when treatment is most effective.
6. What are the treatments?

The treatment of diabetic retinopathy depends on the stage and severity of the condition. In the early stages of non-proliferative diabetic retinopathy (NPDR), treatment may not be necessary, but close monitoring and management of blood sugar levels and blood pressure is important to prevent the condition from worsening.
If diabetic macular edema (DME) is present, the following treatments may be recommended:
- Anti-VEGF injections: These injections are given into the eye to block a protein called vascular endothelial growth factor (VEGF), which can cause abnormal blood vessels to grow and leak in the retina.
- Steroid injections: These injections are given into the eye to reduce inflammation and swelling in the macula.
- Laser photocoagulation: This treatment involves using a laser to seal leaking blood vessels in the retina and reduce swelling in the macula.
In the more advanced stages of proliferative diabetic retinopathy (PDR), treatment may involve:
- Laser photocoagulation: This treatment can be used to shrink and seal abnormal blood vessels in the retina.
- Vitrectomy: This surgical procedure involves removing the vitreous gel from the center of the eye and replacing it with a saline solution. This can help clear any blood or scar tissue that is blocking vision.
It’s important to note that while these treatments can be effective in slowing the progression of diabetic retinopathy and preventing vision loss, they cannot cure the condition. Management of blood sugar levels, blood pressure, and cholesterol levels are also crucial in preventing or slowing the progression of diabetic retinopathy. Regular eye exams are important for monitoring the condition and detecting any changes early on when treatment is most effective.
7. What are the complications of diabetic retinopathy?
Diabetic retinopathy can cause several complications, some of which can lead to severe vision loss or blindness. These complications can include:
- Vitreous hemorrhage: This occurs when the abnormal blood vessels in the retina leak blood into the vitreous gel, which can cause sudden vision loss.
- Retinal detachment: This occurs when the abnormal blood vessels pull on the retina, causing it to separate from the back of the eye. This can cause sudden vision loss and requires emergency treatment.
- Neovascular glaucoma: This occurs when abnormal blood vessels grow on the iris (the colored part of the eye), which can block the flow of fluid out of the eye and increase eye pressure. This can cause severe eye pain, vision loss, and require emergency treatment.
- Macular edema: This occurs when fluid leaks into the macula, which is the part of the retina responsible for central vision. This can cause distorted or blurry vision, and if left untreated, can lead to severe vision loss.
- Blindness: In severe cases of diabetic retinopathy, prolonged or untreated complications can cause permanent vision loss or blindness.
It’s important to manage blood sugar levels, blood pressure, and cholesterol levels to prevent or slow the progression of diabetic retinopathy and its complications. Regular eye exams are also crucial for detecting any changes in the eyes caused by diabetes and preventing vision loss.
8. How do I prevent diabetic retinopathy?
You can help prevent diabetic retinopathy by following these steps:
- Control your blood sugar: Maintaining healthy blood sugar levels is the most important step in preventing diabetic retinopathy. This can be achieved through a healthy diet, regular exercise, and taking medication as prescribed by your healthcare provider.
- Manage your blood pressure: High blood pressure can damage the blood vessels in the eyes and increase the risk of retinopathy. Regular blood pressure checks and medication as prescribed by your healthcare provider can help manage blood pressure levels.
- Control your cholesterol: High cholesterol levels can contribute to the development of diabetic retinopathy. Eating a healthy diet and taking medication as prescribed by your healthcare provider can help manage cholesterol levels.
- Quit smoking: Smoking can damage the blood vessels in the eyes and increase the risk of diabetic retinopathy. Quitting smoking can help reduce this risk.
- Regular eye exams: Having regular eye exams, at least once a year, is important for detecting any signs of diabetic retinopathy early on when treatment is most effective.
- Take care of your overall health: Maintaining a healthy lifestyle, including regular exercise, a healthy diet, and managing stress, can help prevent and manage diabetes and its complications.
By following these steps, you can help prevent or slow the progression of diabetic retinopathy and protect your vision.
9. Is diabetic retinopathy permanent?
The effects of diabetic retinopathy can be permanent, especially if the condition is left untreated or if complications occur. In the early stages of retinopathy, if blood sugar levels and blood pressure are well-managed, and treatment is provided when necessary, it’s possible to prevent or slow the progression of the condition and protect vision.
However, in more advanced stages of diabetic retinopathy or if complications occur, vision loss can be permanent. This is why it’s crucial to have regular eye exams to detect any changes in the eyes caused by diabetes and to seek treatment promptly if needed.
It’s also important to manage blood sugar levels, blood pressure, and cholesterol levels to prevent or slow the progression of diabetic retinopathy and its complications. By taking care of your overall health and following your healthcare provider’s recommendations, you can help protect your vision and reduce the risk of permanent vision loss.
10. Why you need to visit Vijaya Nethralaya eye hospital for diabetic retinopathy?
If you have diabetes, it’s important to have regular eye exams to detect any changes in your eyes caused by the condition, including diabetic retinopathy. Vijaya Nethralaya is an eye hospital that specializes in treating a range of eye conditions, including diabetic retinopathy. The hospital has a team of experienced ophthalmologists who can provide a comprehensive evaluation of your eyes and develop a personalized treatment plan based on your specific needs.
Vijaya Nethralaya offers state-of-the-art diagnostic and treatment technologies, including retinal imaging, laser treatments, and vitreoretinal surgery, to manage retinopathy and its complications. They also provide education and support to help you manage your diabetes and maintain a healthy vision.
If you have diabetes and are experiencing vision changes or have not had an eye exam in a while, it’s important to schedule an appointment with an eye doctor or a hospital like Vijaya Nethralaya for a comprehensive eye exam. Early detection and treatment of diabetic retinopathy can help preserve your vision and prevent vision loss.