Micro Invasive Glaucoma Surgeries (MIGS): Innovations in Glaucoma Treatment
Introduction to Micro Invasive Glaucoma Surgeries (MIGS)
- MIGS is a newer angle surgery performed nowadays to reduce intraocular pressure in mild to moderate open-angle glaucoma.
- Angle is a circumferential area that lies at the junction of the cornea (transparent front part of eyes) and the iris (brown part) through which the fluid in the anterior chamber drains out of the eye.
- It is visualized as a light-to-dark brown structure through a gonioscopy lens.
- All MIGS procedure targets this drainage angle, either by removing the trabecular meshwork, which is a sieve-like structure covering the Schlemm’s canal, or bypassing the trabecular meshwork by implanting a stent so that the stent lets the fluid flow unidirectionally out of the eye.
- It is a suture-less procedure that can be performed quickly under local anesthesia with the help of a specially designed intraoperative direct gonioscopy lens.
- It can either be done as a standalone procedure or combined with cataract surgery.
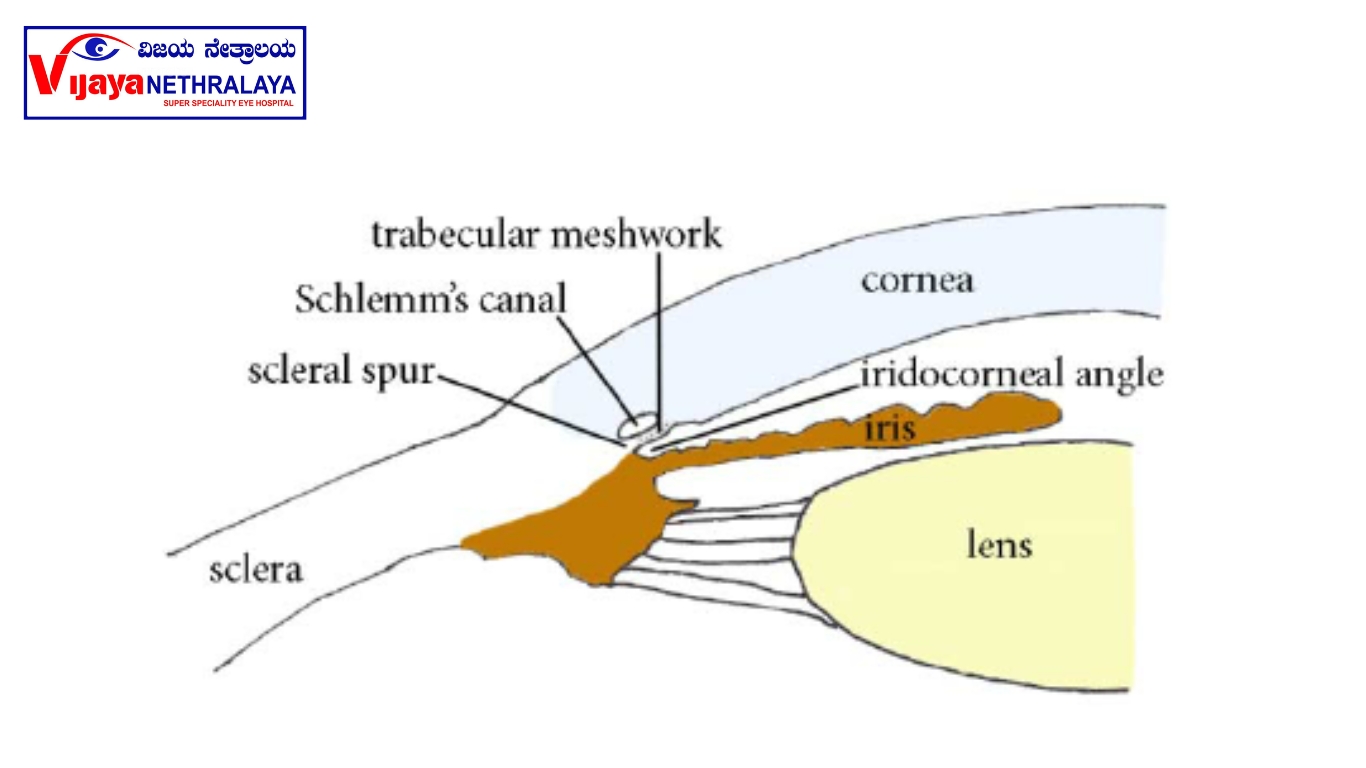
- Angle is a circumferential area that lies at the junction of the cornea (transparent front part of eyes) and the iris (brown part) .
- Postoperatively, IOP is reduced by around 20-25% from baseline and there is a reduction of the number (1-2) of anti-glaucoma medications (AGM) used.
Kahook Dual Blade (KDB) Glaucoma Surgery: A Breakthrough in Treating Glaucoma:
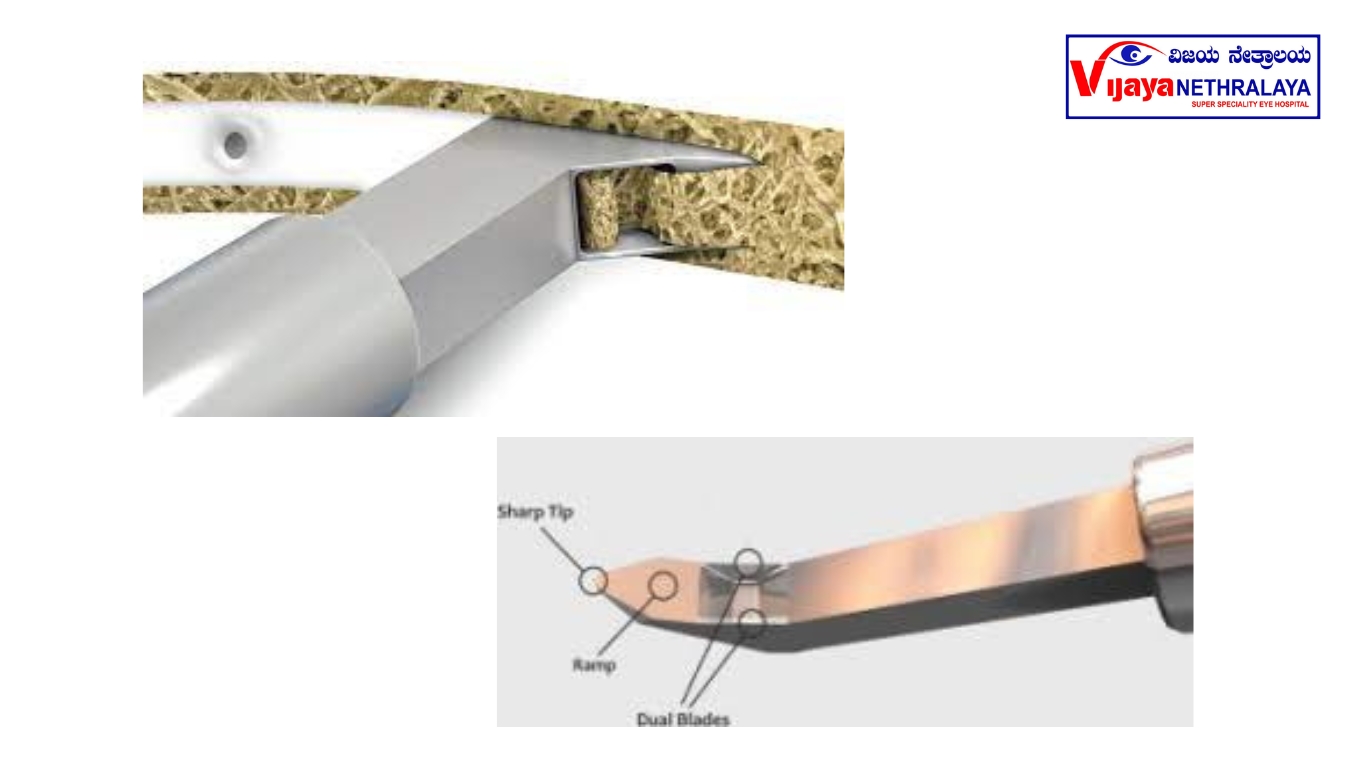
- It is a specially designed device for single use, to excise trabecular meshwork. It is entered into the eye through a clear corneal microincision.
- The device is made up of surgical-grade stainless steel and is designed specifically to fit in the scheme’s canal. It has a long and thin shaft that allows access to the anterior chamber, a sharp pointed tip to pierce the trabecular meshwork, a ramp that stretches and lifts the eye tissue, and the tissue is cut simultaneously cut on either side using the dual blade. This entire process is smooth and any damage to the canal is prevented by the footplate.
What is IStent glaucoma surgery?
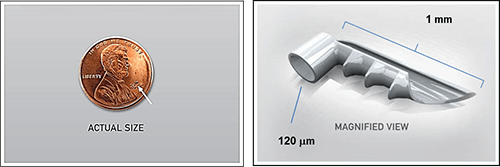
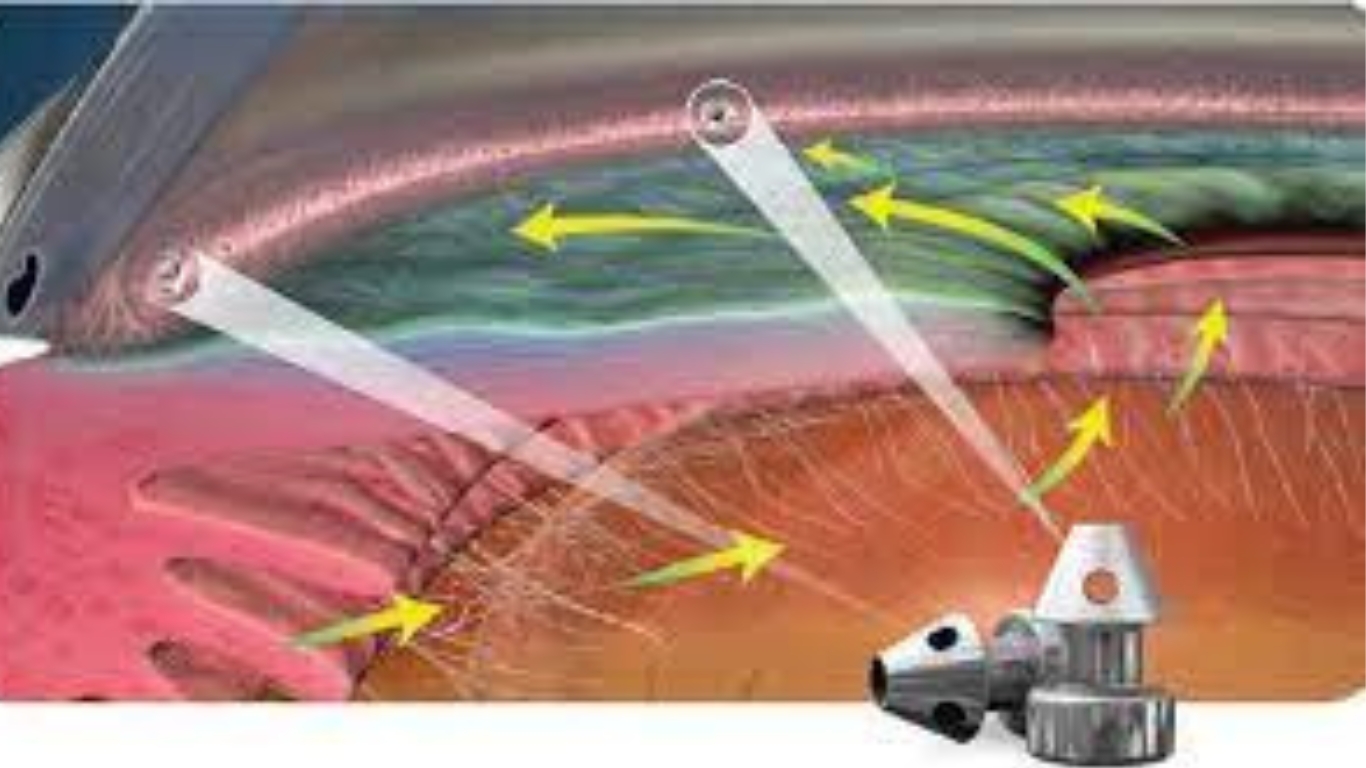
it is the smallest implantable device, made up of titanium, which is implanted through the trabecular device into the canal of schlemm to enhance the fluid outflow and to lower intraocular pressure.
ISTENT 2 nd GENERATION
Advantages Of MIGS:
1)Highly safe and effective, 2) Faster recovery rate, 3) Minimal trauma to the surrounding tissues, 4) The conjunctiva is preserved for future glaucoma surgeries, 5) There is a reduction in the use of the number of AGM, 6) It can be combined with cataract surgery, 7) This procedure does not create a bleb, as the fluid is routed through physiological pathways.
Ideal candidates for MIGS:
1) Primary and secondary open angle glaucoma patients with mild to moderate disease
2) Patients who are non-compliant or intolerant with anti-glaucoma medications
3) Patients who have primary ocular surface disease or secondary to chronic AGM use /
preservative toxicity
4) Patients who are not able to come for frequent postoperative follow-ups as required in case of
traditional incisional glaucoma surgeries
Complications with MIGS procedure:
- Possibility of micro bleeding during surgery with spontaneous resolution in post-operative
period. - Since glaucoma is a progressive disease, the patient is expected to continue anti-glaucoma eyedrops
if target IOP is not achieved or when progression is noted.
Our Glaucoma Specialists: Leaders in the Field of Glaucoma Care

Dr. Thanemozhi
MBBS, DO, DNB (OPHTHAL), FGRGUHS, FAICO(GLAUCOMA)

Dr. Ravina Todi
MBBS, MS(Ophthalmology), Fellowship in Glaucoma
Conclusions:
Over the years, there have been limited options for mild to moderate glaucoma disease. To fill this gap, MIGS has been introduced. This has proven to be effective in reducing IOP in those cases.