Laser Peripheral Iridotomy: Preventing Glaucoma, Changing Lives
Laser Peripheral Iridotomy:
An iridotomy is a small hole created with the laser beam in the iris (colored part of the eye). The iridotomy allows
fluid to circulate freely within the eye, minimizing the risk of a sight-threatening pressure rise.
A laser peripheral iridotomy is performed to treat or prevent a sudden rise in pressure inside the eye due to
narrow angles, narrow-angle glaucoma, or acute angle closure glaucoma. This is generally done in the far edge
(periphery) of the iris to help open the drainage angle and the hole is not visible to the naked eye.
Why You May Need This Procedure:
Symptoms of an Angle Closure Attack:
- To prevent an attack of acute glaucoma
- To treat an attack of acute glaucoma
- To treat chronic glaucoma where the drainage channel is very narrow
- Hazy or foggy vision
Severe eye and/or brow pain - Headache, nausea, vomiting
- Seeing rainbow-colored rings or
- Halos around lights
An acute angle-closure glaucoma attack is an emergency. It must be treated quickly to prevent loss of vision. Some people do not have symptoms with their closed-angle glaucoma, but high pressure is still damaging the optic nerve. This is called chronic angle-closure glaucoma . This condition often requires surgery.
Understanding Narrow-Angle and Angle Closures:
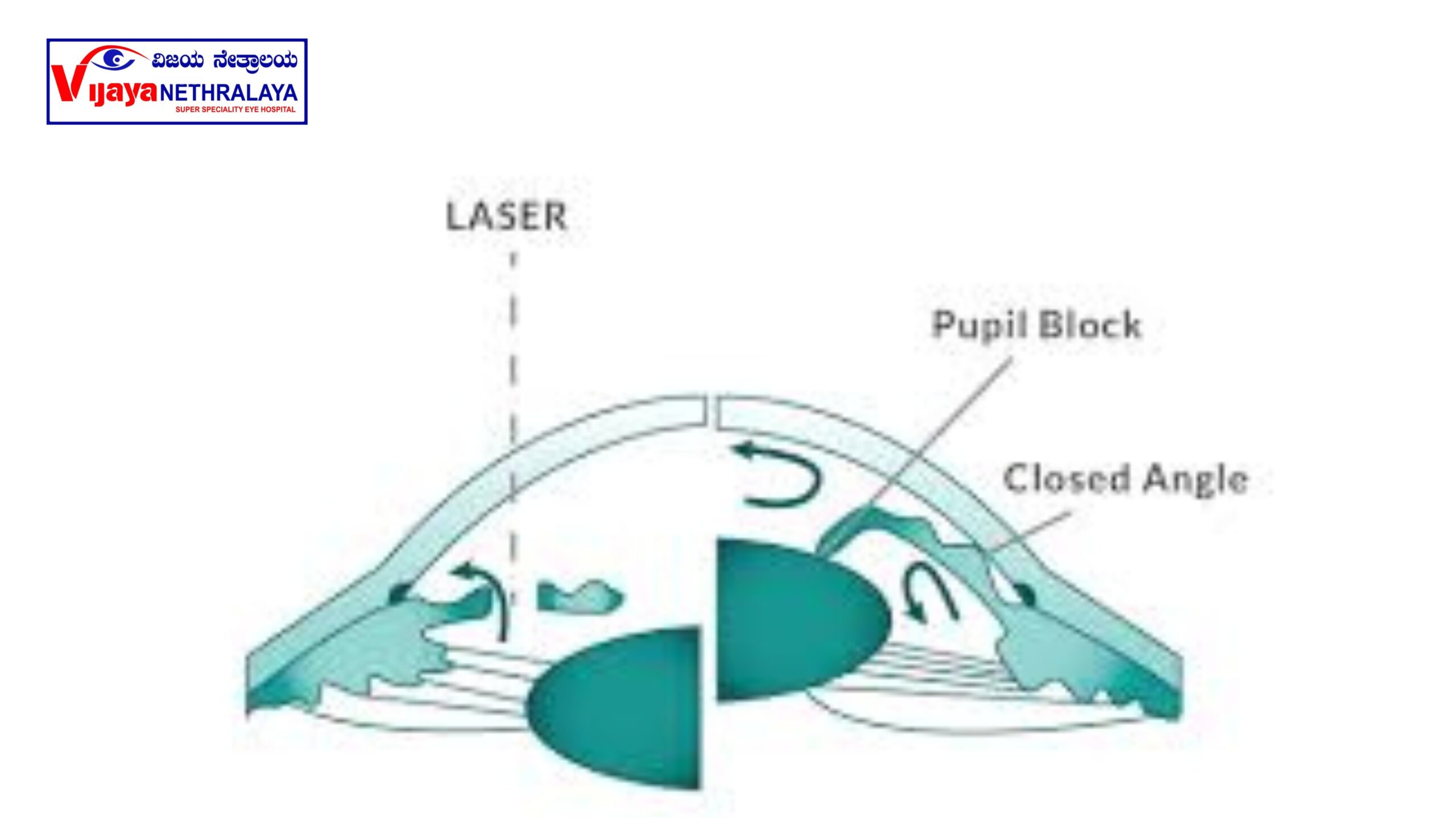
The pressure in each eye is kept at the level of fluid coming into the eye. It flows in behind the iris, then forward through the pupil, and leaves the eye in the ‘angle’ - the gap between the edge of the iris and the clear window at the front of the eye (cornea).
Angle-closure glaucoma is when the iris completely blocks fluid (called aqueous humor) from leaving the front of the eye. This is a serious problem that can cause high pressure inside the eye (intraocular pressure), which can be painful and can cause permanent damage to the optic nerve and permanent vision loss within a few days.
Laser iridotomy helps fluid drain properly again, lowering your eye pressure. Laser iridotomy is also used to prevent angle-closure glaucoma in people who are at risk of having this problem. These people have what is called a “narrow-angle.”
If the iris suddenly blocks the drainage angle, it is called an attack of acute angle-closure glaucoma.
Understanding the Procedure of Laser Peripheral Iridotomy:
It is an outpatient procedure and normally takes approximately 15-30 minutes. On arrival, doctor will explain the
procedure and ask you to sign a consent form. Nurse will then put eye drop pilocarpine 2% to make the pupil
small for better visualization of iris crypts, where the laser is to be performed. Anesthetic drops are applied. The
procedure is performed with a special contact lens . During the procedure, you will see some bright flashes of
light, hear a clicking noise and may feel slight discomfort as the laser is fired into the sensitive tissue of the iris.
Laser shots are delivered to create a hole in the peripheral iris to allow aqueous to flow thoroughly.

Post-Treatment Expectations of Laser Peripheral Iridotomy:
Your eye may become pink and sore and the vision is often disturbed for the rest of the day. For this reason patients are strongly advised not to drive home. You may be prescribed steroid drops for a few days to control any inflammation and sometimes drops and /or tablets to bring the eye pressure back to normal.In severe cases, patients may need to have the eye pressure checked a few hours after treatment.
Understanding the Side Effects of Laser Peripheral Iridotomy:
The side effects after YAG Laser PI are mild, uncommon and short-lived:
- Redness, light sensitivity, and discomfort for a few days after the procedure.
- Short-lived increase in eye pressure.
- Temporary blurred vision.
- Temporary inflammation.
- A small amount of Hemorrhage from the laser hole (inside the eye) is fairly common, and can cause
misty vision, which usually settles within 24 hours. - Cystoid macular oedema can occur and can be more frequent in diabetic patients. This is a swelling in
the retina at the back of the eye which can be treated successfully with drops in most cases. - In general, only less than 1% of people find their vision deteriorates following the procedure and some
may experiencing glare. - Whilst one treatment is usually enough, we may recommend further laser treatment at a later date if the
laser hole is not large enough or if it close up. If this is the case, we will have to repeat the treatment at
a later date.
The Benefits of Laser Peripheral Iridotomy in Glaucoma Management
- Aims to prevent raised intraocular pressure and
reduce the risk of vision loss from glaucoma. - If the procedure is performed at an early stage of
the disease, there is a 66–75% chance of
preventing further progression. - It will not restore any sight you may have already
lost; neither will it improve your sight. - The laser treatment is to prevent a sudden (acute)
rise in pressure within your eye. Without having this
treatment, you are at risk of developing sudden glaucoma and irreversible blindness.
