Cataract Surgery for Diabetics: Ensuring Clear Vision and Optimal Outcomes
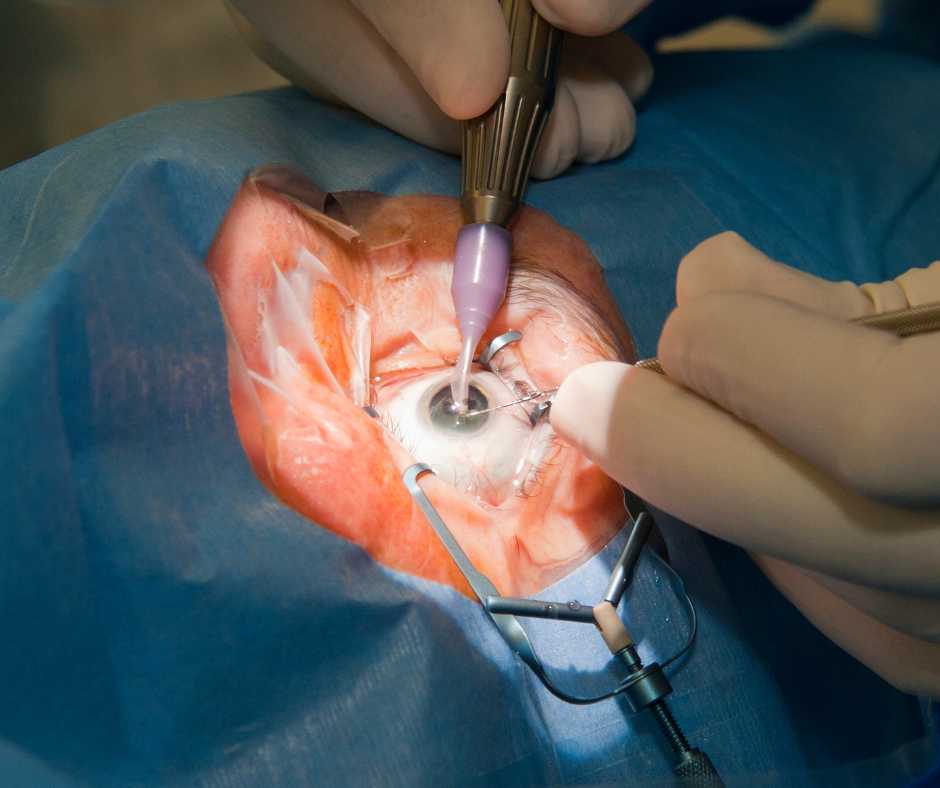
Cataract surgery for diabetics are a common vision problem that affects people of all ages, including those with diabetes. cataract surgery for Diabetes can accelerate the development and progression of cataracts, leading to impaired vision and reduced quality of life. However, with advancements in surgical techniques and careful management, cataract surgery for diabetics can yield successful outcomes and improved vision.
In this blog, we will explore the relationship between diabetes and cataracts. The unique considerations for cataract surgery in diabetic patients, and the steps involved in ensuring a safe and successful procedure.
Understanding the Link between Diabetes and Cataracts:
How diabetes influences cataract development and progression
Diabetes can significantly influence the development and progression of cataracts, leading to vision impairment and potential complications. Understanding the relationship between diabetes and cataracts is crucial for effectively managing these conditions.

Here are some key points explaining how diabetes influences cataract development and progression:
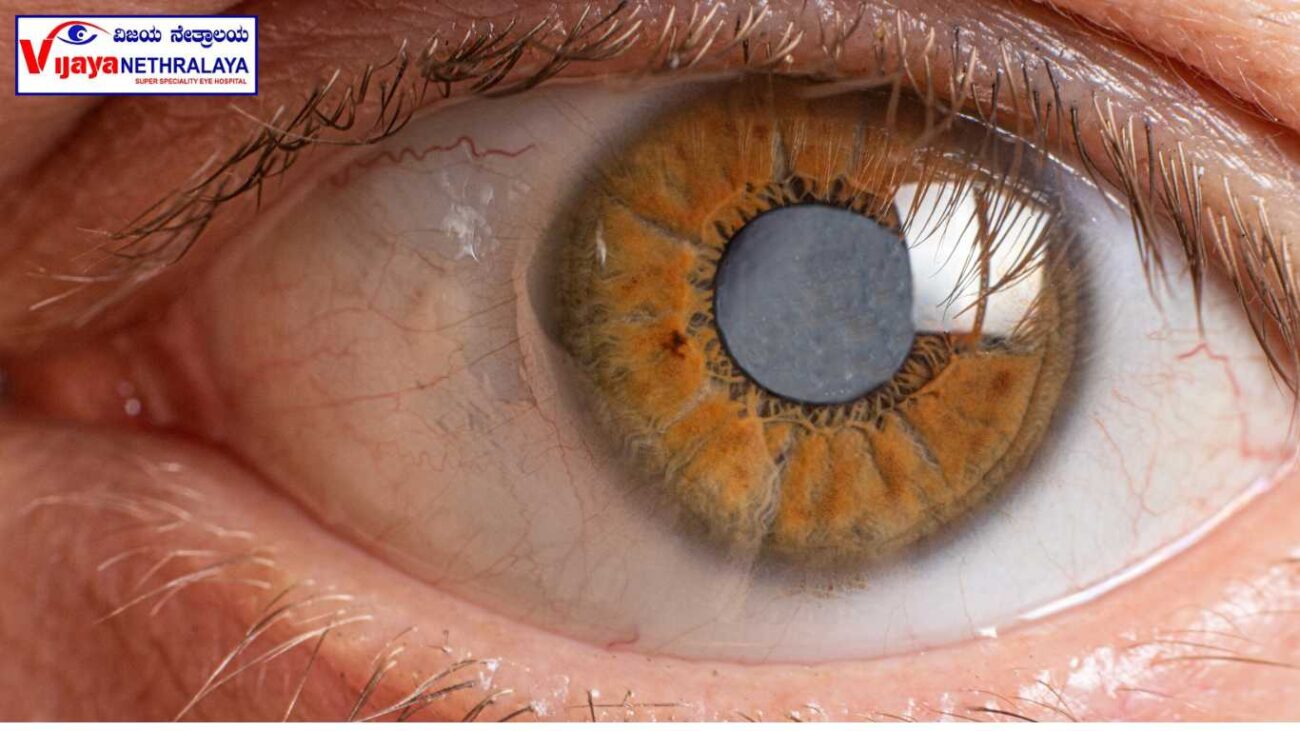
- Accelerated formation: Diabetes can accelerate the formation of cataracts, causing them to develop at an earlier age compared to non-diabetic individuals. High blood sugar levels characteristic of diabetes can lead to increased sorbitol accumulation within the lens of the eye. altering its structure and impairing its transparency. This process contributes to the formation of cataracts.
- Increased oxidative stress: Diabetes is associated with increased oxidative stress throughout the body, including the eye. Elevated levels of blood glucose can lead to the production of reactive oxygen species (ROS) and free radicals. This oxidative stress contributes to the development and progression of cataracts.
- Impaired antioxidant defense mechanisms: Diabetic individuals may have impaired antioxidant defense mechanisms, making them more susceptible to oxidative damage. Antioxidants play a crucial role in neutralizing the harmful effects of oxidative stress. However, in diabetes, the reduced levels of antioxidants can further exacerbate the damage to the lens, accelerating cataract formation.
- Altered fluid balance: Diabetes can disrupt the delicate fluid balance within the lens. Normally, the lens maintains a balance of fluid and transparency. However, in diabetes, increased levels of glucose in the lens can lead to the osmotic movement of water into the lens, causing swelling and altering its optical properties. This fluid imbalance can contribute to the development and progression of cataracts.
- Aggravated diabetic complications: Diabetic individuals often have concurrent complications, such as diabetic retinopathy and macular edema. These conditions can exacerbate the impact of cataracts on vision. The presence of diabetic retinopathy is characterized by abnormal blood vessels in the retina. can complicate cataract surgery and increase the risk of postoperative complications. your Doctor will take suitable measures to prevent this.
CALL NOW
Identifying diabetic cataracts Signs and symptoms:
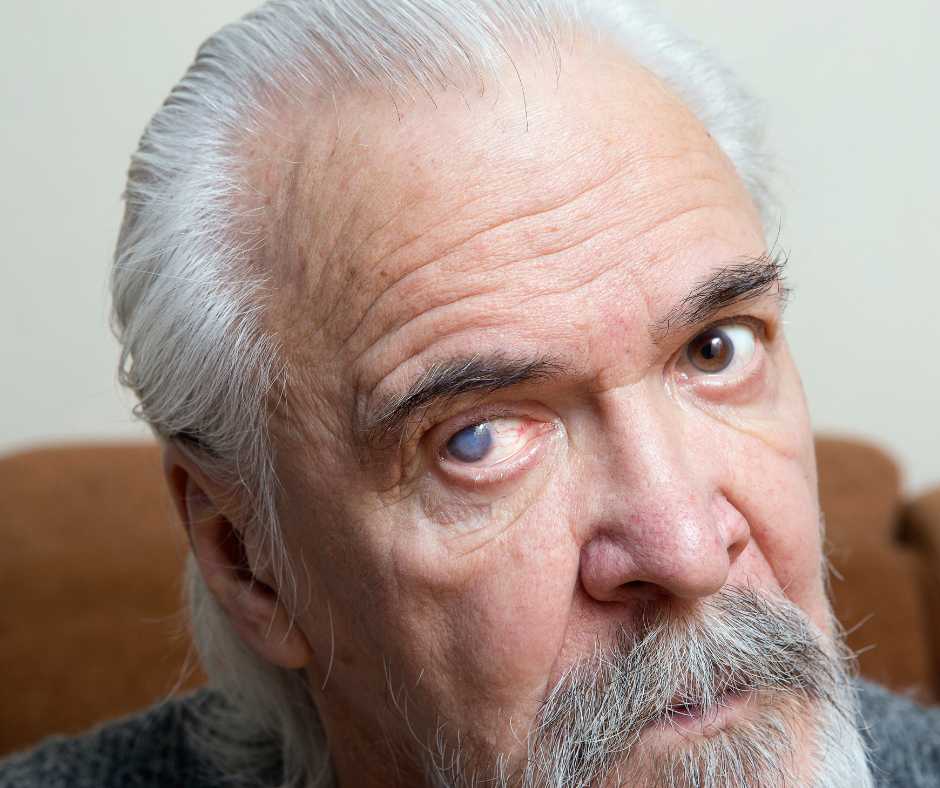
Identifying diabetic cataracts relies on recognizing the signs and symptoms that distinguish them from cataracts in non-diabetic individuals. As diabetes can influence the characteristics and progression of cataracts, understanding these specific indicators is crucial. Here are some common signs and symptoms to help identify diabetic cataracts:
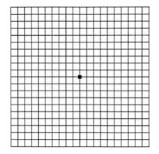
- Blurred or cloudy vision: Diabetic cataracts can cause a gradual decline in vision clarity. Individuals may experience blurred or hazy vision, as if looking through a foggy or cloudy lens. This can affect both near and distance vision.
- Increased sensitivity to light: Diabetic cataracts may cause individuals to become more sensitive to bright lights or glare. They may experience discomfort or find it challenging to see clearly in well-lit environments or when exposed to intense light sources.
- Altered color perception: Some diabetic individuals with cataracts may notice a change in their perception of colors. Colors may appear dull, faded, or less vibrant than they once were. This can affect the ability to differentiate between shades and hues.
- Difficulty with night vision: Diabetic cataracts can impair night vision, making it challenging to see in low-light conditions or darkness. Individuals may experience increased difficulty driving at night or navigating dimly lit areas.
- Frequent changes in eyeglass prescription: As diabetic cataracts progress, the refractive power of the eye can change rapidly. This may result in the need for frequent adjustments to eyeglass prescriptions. If an individual’s vision worsens noticeably and requires frequent updates to their corrective lenses, it may be indicative of cataracts.
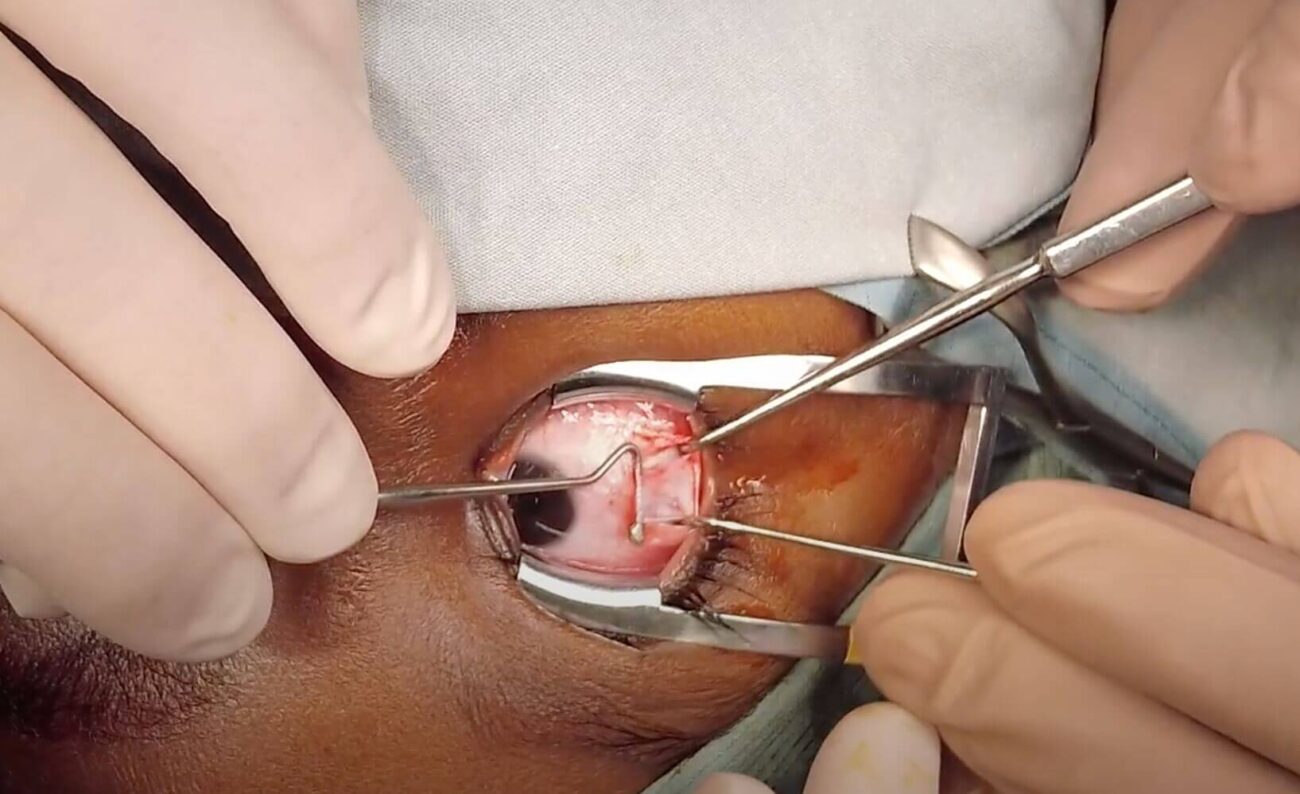
Preoperative Preparations and Assessment:
- Collaborative approach: Coordinating with the ophthalmologist and endocrinologist
- Evaluating diabetic control: Assessing blood glucose levels and HbA1c
- Addressing diabetic complications: Managing retinopathy and macular edema
- Optimizing overall health: Controlling blood pressure and cholesterol levels
- Medication management: Adjusting diabetes medications before surgery
Postoperative Care and Recovery:
- Immediate post-surgical care: Monitoring blood glucose levels and medications.
- Vision recovery timeline: What to expect during the healing process.
- Medication adherence: Administering postoperative eye drops and managing diabetes medications.
- Follow-up visits: Regular check-ups with the ophthalmologist and endocrinologist.
- Lifestyle adjustments: Incorporating healthy habits to maintain optimal eye and overall health.
Conclusion:
Cataract surgery for diabetics requires a comprehensive approach, considering both the individual’s ocular health and their diabetic control. With proper preoperative preparations, meticulous surgical techniques, and attentive postoperative care, diabetic patients can achieve successful cataract surgery outcomes and restored vision. It is crucial for patients with diabetes to collaborate closely with their ophthalmologist and endocrinologist throughout the process, ensuring optimal management of both their eye health and diabetes. By understanding the unique considerations and potential challenges involved, diabetic individuals can make informed decisions and take proactive steps to safeguard their vision and overall well-being.
Author Details:

Dr. Sushruth Appajigowda is a well-known Cornea, Cataract, and LASIK Surgeon in Bangalore, and the chief Cataract and Refractive surgeon at Vijaya Nethralaya Eye Hospital, Nagarbhavi Bangalore. Known as one of the best LASIK surgeons in the country, he has over 12+ years of experience with multiple platforms of LASIK like ZEISS, ALCON, SCHWIND, AMO, and Bausch and Lomb. He has conducted over 5000 LASIK. Dr Sushruth is a Certified Refractive Surgeon and Fellow of All India Collegium Of Ophthalmology. He is recognised speaker in various National and International Forums. His expertise lies in choosing the right type of procedure for you based on your health requirement. You can schedule an appointment by scanning the QR Below or clicking the link below the QR and say bye to glasses forever!










https://yct.su/terijoki/pages/promokod__260.html 1хбет промокод бонус
https://www.aviator-game-bonus.com/ Aviator Game Play Online