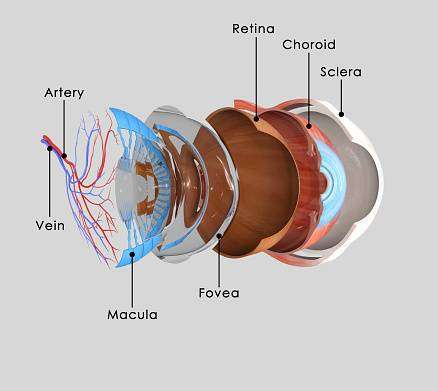
Basic Understanding of Eyeball Anatomy
The eye is shaped like a ball with three layers and gel-filled inside the cavity. Outermost is
the sclera, the innermost is the retina and the middle layer is called the uveitis.
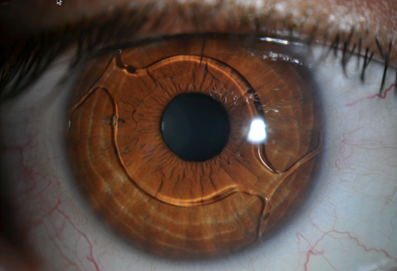
When uvea becomes inflamed i.e. red and swollen the condition is called uveitis.
As uvea contains a lot of blood vessels that nourish the eye, the inflammation affects
other vital parts like cornea, retina, sclera, etc.
What are the Types of Uveitis?
The type depends on which part of the eye is inflamed;
- Iritis(anterior uveitis) affects the front of your eye.
- Cyclitis(intermediate uveitis) affects the ciliary body.
- Choroiditis AND Retinitis (posterior uveitis) affect the back of the eye.
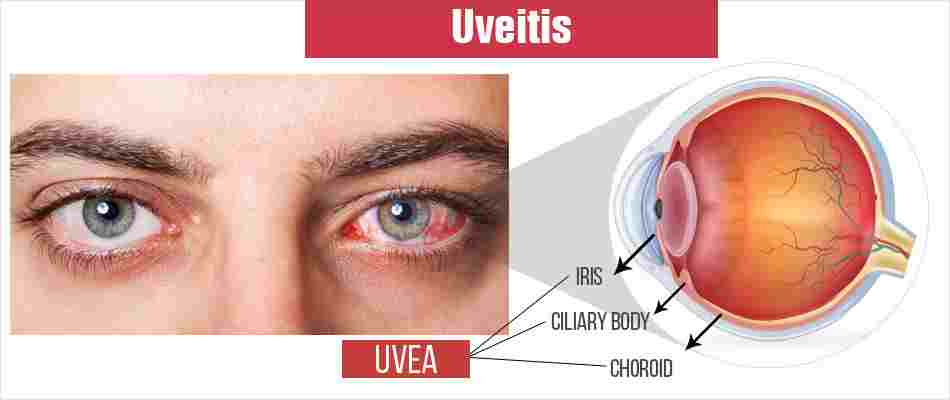
Autoimmune uveitis Symptoms:

The patient describes their symptom as;
- Eye Redness
- Blurring of vision
- Floating spots in the field of vision (floaters)
- Sensitivity to light.
- Some experience feelings of eye pain/pressure building up inside the eye.
- Vision drop could be both mild and severe
uveitis cause:

There are many causes; Frequent causes include;
- Injury to the eye
- Infection, such as the herpes virus, chicken pox virus, TB, syphilis
- Autoimmune or inflammatory disorder. such as lupus, IBD, and rheumatoid arthritis. It is often difficult to ascertain the cause, which can be very costly.
- Also it may be caused by a bruise or diseases like AIDS, multiple sclerosis, arthritis, syphilis, and tuberculosis.
What is the Difference Between Infection and Inflammation?
Infection refers to the invasion and multiplication of bacteria or viruses within the body while inflammation is a protective response against the pathogen. When inflammation happens chemicals from your body’s white blood cells enter the blood and tissues to fight the invaders. As this inflammation progresses it could damage your arteries, organs, and joints.
What are the treatments:
The treatment depends on the cause of uveitis.
- Iritis is often treated with anti-inflammatory eye drops.
- Chronic forms of uveitis may require immunomodulatory drugs.
- In some non-infectious causes, one may choose to treat with local injections around the eye.
- If the workup done for you has revealed a particular cause, then you will receive treatment for that. If no cause is revealed then the treatment is with anti-inflammatory topical and oral medication.
Close Follow-up with Your Doctor is Important!
Sometimes your doctor may refer you to a rheumatologist or pulmonologist doctor
depending on the cause. We strongly recommend that anyone with the ocular inflammatory
disease be treated by an ophthalmologist who has completed a fellowship in uveitis. It
could be a difficult illness to diagnose.
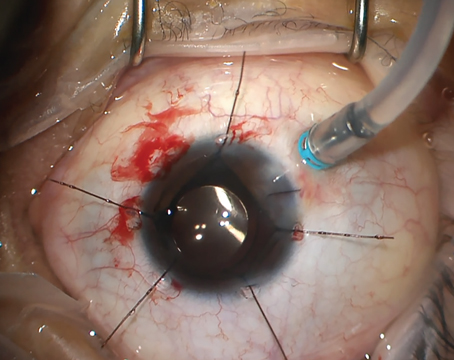
Uveitis Diagnosis:
The healthcare provider caring for your eyes will look at the inside of your eye during an eye exam. A standard eye exam usually includes:
- Visual acuity test (reading eye charts) to check for vision loss.
- Ocular pressure test (tonometry) to measure pressure inside the eye.
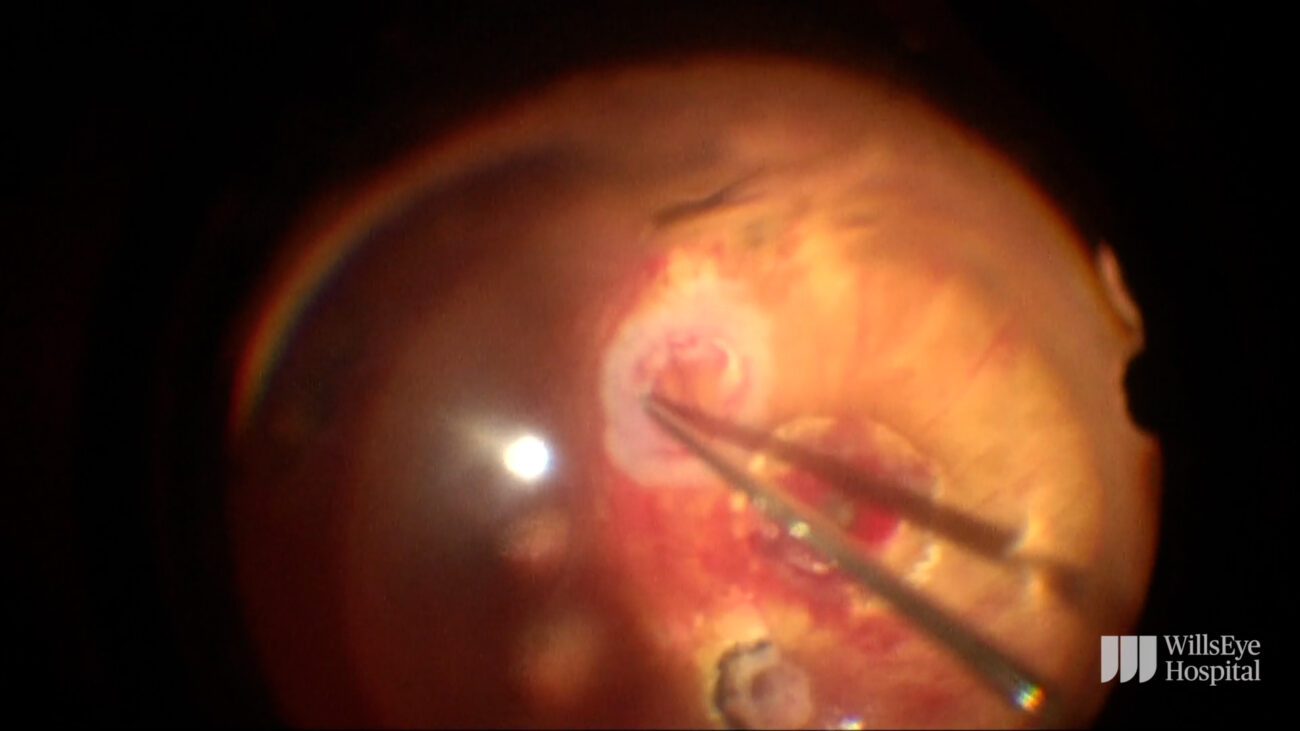
- Slit-lamp exam to examine the inside of the eye with a special microscope called a slit lamp.
- Dilated eye exam to widen pupils so your healthcare provider can look inside your eyes using a special lens.
Your healthcare provider may also order other tests, such as:
- Blood tests to rule out infections or underlying autoimmune diseases.
- Imaging your chest or brain to looking for systemic inflammatory causes.
- Fluorescein angiography to get images of blood vessels in the back of the eye.
- Gonioscopes to examine the front of the eye where the liquid drains.
- Blood tests to rule out infections or underlying autoimmune diseases.
- Imaging your chest or brain to looking for systemic inflammatory causes.
- Fluorescein angiography to get images of blood vessels in the back of the eye.
- Gonioscopes to examine the front of the eye where the liquid drains.
- Optical coherence tomography (OCT) to get detailed images of the back of the eye, including the retina.
- Optical coherence tomography angiography (OCTA) to produce 3D images of blood flow through the eye.
- Visual field test to check for damage to the optic nerve that may affect your ability to see things off to the side (peripheral vision).
- To get detailed images of the back of the eye, including the retina.
- Optical coherence tomography angiography (OCTA) to produce 3D images of blood flow through the eye.
- Visual field test to check for damage to the optic nerve that may affect your ability to see things off to the side (peripheral vision).
At Vijaya Nethralaya Super Speciality Eye Hospitals some doctors have specialized in treating Uveal diseases. Utmost care is taken to control the disease at an early stage and the patient is given the best treatment possible to safeguard his/her vision.
Complications/Problems are Arises:
If you don’t seek prompt medical treatment you’re at an increased risk of developing complications that could lead to vision loss. These problems can include:
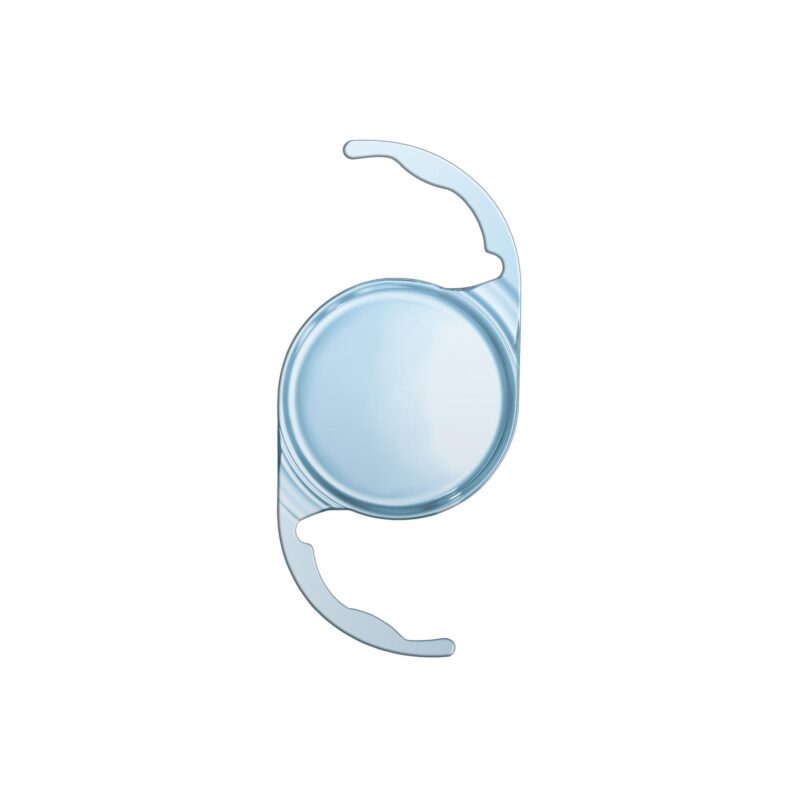
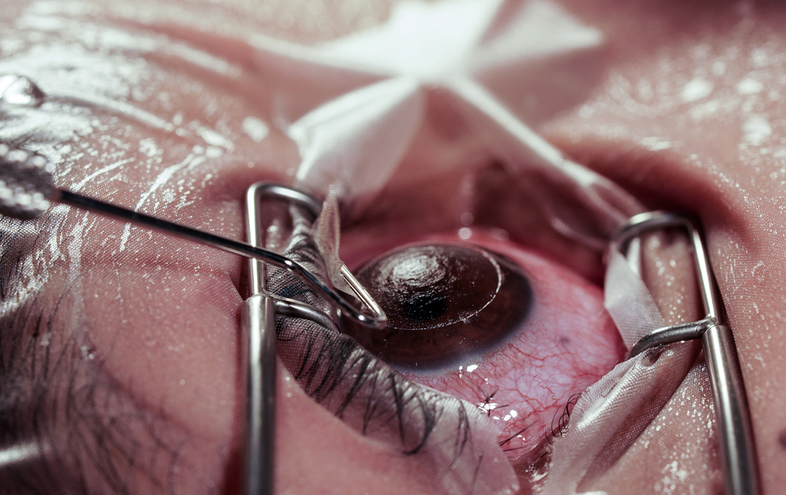
- Cataracts
- Glaucoma
- Inflammation of the gel-like fluid in your eye (vitreous)
- Retinal inflammation (retinitis)
- Swelling in the back of your eye (macular edema)
- Calcium accumulation on your cornea (band keratopathy)
- Attachment of your iris to your lens this can result in adhesions, causing your pupil to irregular
Risk factors:
Several factors can increase a person’s risk of developing uveitis. Some common risk factors are:
- smoking
- use of certain medications
- vitamin D levels
- living with an autoimmune disease, such as rheumatoid arthritis
- pregnancy
In addition, females have a higher chance of developing uveitis than males.
How long does blurred vision last with uveitis?
With treatment, uveitis may clear up in as little as 2-5 weeks although depending on the severity, it may take several months to resolve.
How I cured my uveitis?
Treatment only suppresses the harmful inflammation until the disease process is stopped by your body’s own healing process. The treatment needs to be continued as long as the inflammation is active.
Continue Reading:
About author :

Dr. Mansi Mehrotra is Medical Retina And Uvea Consultant Ophthalmologist at Vijaya Nethralaya, Bangalore. With a special interest in diabetic retinopathy and age-related macular degeneration, Dr. Mansi has performed several cataract surgeries throughout her career. She has also treated retinopathy of prematurity with a laser indirect ophthalmoscope. When it comes to academics, she has penned several publications for peer-reviewed journals and presented papers at state conferences.