Introduction
Pneumatic retinopexy is a specialized surgical procedure that treats retinal detachment, a potentially sight-threatening condition. This innovative technique utilizes a gas bubble to reposition the retina and seal tears, offering a minimally invasive alternative to traditional retinal surgeries. It is particularly suitable for select patients with specific types of detachment, providing a faster recovery and reduced surgical complexity. Understanding the indications, procedure, and postoperative care of pneumatic retinopexy is essential for ensuring successful outcomes and preserving vision.
What is Pneumatic Retinopexy?
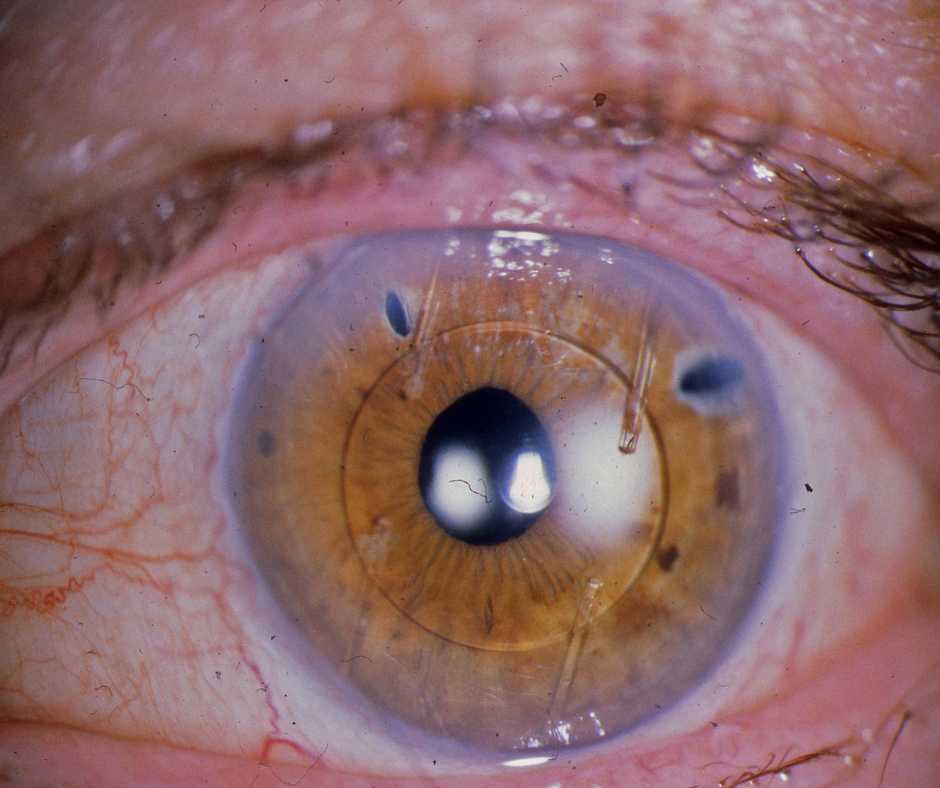
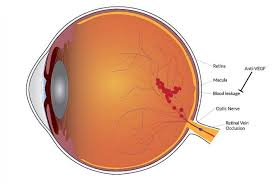
Pneumatic retinopexy is a minimally invasive surgical procedure that treats certain types of retinal detachment. The retina, a light-sensitive layer at the back of the eye, can detach due to tears or holes, leading to vision loss. This procedure involves injecting a gas bubble into the vitreous cavity (the gel-like substance inside the eye) to push the detached retina back into position. Once the retina is reattached, additional treatments like laser photocoagulation or cryopexy are applied to seal the tear and prevent further detachment. Pneumatic retinopexy offers a quicker and less invasive alternative to other retinal surgeries, such as scleral buckling or vitrectomy.
Types of Pneumatic Retinopexy
The procedure can be categorized based on the type of gas used to create the bubble:
- Perfluoropropane (C3F8):
- A long-acting gas that expands within the eye and remains for several weeks.
- Suitable for larger or more complex detachments due to its extended duration.
- Sulfur Hexafluoride (SF6):
- A shorter-acting gas that typically lasts for 1-2 weeks.
- Ideal for smaller or simpler retinal detachments, allowing for quicker recovery.
Indications
Pneumatic retinopexy is indicated for patients with:
- Retinal detachments caused by a single break or a small group of breaks.
- Tears or holes located in the upper two-thirds of the retina.
- Minimal or no proliferative vitreoretinopathy (PVR), a condition where scar tissue complicates reattachment.
- Patients who are medically fit and able to maintain specific head positioning post-surgery.
Contraindications
This procedure may not be appropriate for:
- Retinal detachments involving multiple or large tears.
- Tears located in the lower third of the retina, as the gas bubble may not adequately reach these areas.
- Significant PVR, which makes the retina difficult to reattach.
- Vitreous hemorrhage or intraocular inflammation.
- Patients unable to comply with postoperative positioning or follow-up care.
Advantages
- Minimally invasive: The procedure involves no large incisions, reducing surgical trauma.
- Outpatient procedure: Patients can go home the same day after the procedure.
- Quick recovery: Compared to other methods, the recovery period is shorter.
- Cost-effective: More affordable compared to scleral buckling or vitrectomy.
Disadvantages
- Limited scope: Only suitable for specific types of retinal detachment.
- Strict postoperative requirements: Success depends on the patient’s ability to maintain precise head positioning.
- Risk of complications: Potential for increased intraocular pressure, gas migration, or the need for additional surgery.
Patient Selection
Selecting the right patients is essential for the success of pneumatic retinopexy. Ideal candidates include:
- Patients with a single or a small group of retinal tears.
- Individuals with tears located in the superior retina.
- Those who can maintain strict head positioning after the procedure.
- Patients without advanced PVR or media opacities such as significant cataracts or vitreous hemorrhage.
Surgical Procedure
The surgical steps for pneumatic retinopexy are meticulously planned to ensure optimal outcomes.
Gas Selection
The choice of gas depends on the extent and location of the detachment:
- C3F8 (Perfluoropropane): Best for larger or more complex tears due to its extended duration.
- SF6 (Sulfur Hexafluoride): Preferred for simpler cases requiring shorter recovery times.
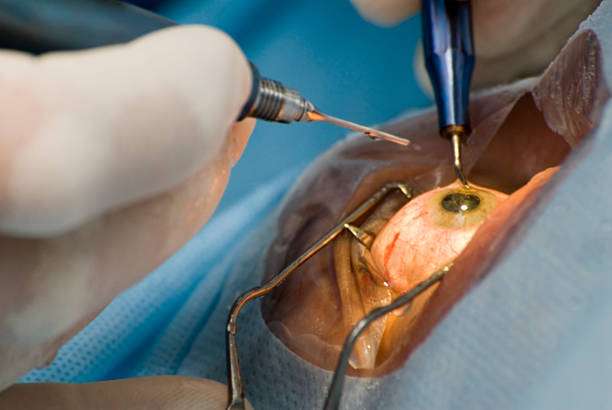
Operative Procedure
- reparation: The doctor cleans and numbs the eye with topical or local anesthesia.
- Cryopexy or Laser Photocoagulation: The surgeon seals retinal tears with cryotherapy or laser to prevent fluid reaccumulation.
- Gas Injection: The doctor injects a small amount of sterile gas into the vitreous cavity using a fine needle.
- Head Positioning: The patient positions their head to allow the gas bubble to press against the detached retina.
- Additional Sealing: The doctor may apply laser or cryotherapy during follow-up to reinforce the seal.
Why Might I Need Pneumatic Retinopexy?
Pneumatic retinopexy is recommended for specific cases of retinal detachment to:
- Prevent permanent vision loss.
- Offer a less invasive alternative to more complex surgeries.
- Treat detachments in patients who are not candidates for scleral buckling or vitrectomy.
What Are the Risks of Pneumatic Retinopexy?
While generally safe, the procedure carries some risks, including:
- Failure to reattach the retina, necessitating further surgery.
- Increased intraocular pressure, which may lead to glaucoma if untreated.
- Cataract formation due to gas bubble contact with the lens.
- Infection, bleeding, or inflammation.
- Migration of the gas bubble to unintended areas, such as the anterior chamber.
How Do I Get Ready for Pneumatic Retinopexy?
Preparation involves:
- A thorough eye examination, including ultrasound imaging to assess the detachment.
- Discussion of postoperative care requirements, including head positioning.
- Adjusting medications as instructed by your ophthalmologist.
What Happens During Pneumatic Retinopexy?
The procedure typically involves the following steps:
- The eye is numbed with anesthesia.
- A gas bubble is carefully injected into the vitreous cavity.
- Retinal tears are sealed using laser or cryopexy.
- Postoperative instructions, particularly regarding head positioning, are provided to the patient.
What Happens After Pneumatic Retinopexy?
Postoperative care includes:
- Maintaining proper head positioning to ensure the gas bubble remains in contact with the retinal tear.
- Applying prescribed eye drops helps prevent infection and reduce inflammation.
- Attending regular follow-up visits to monitor healing and intraocular pressure.
Complications
Possible complications include:
- Anterior Hyaloidal Gas: Gas bubble migration into the anterior hyaloid region, potentially affecting vision.
- Subretinal Gas: Gas entering the subretinal space, complicating reattachment.
- Gas in the Anterior Chamber: Migration of gas into the anterior chamber, which can increase intraocular pressure.
Postoperative Care
- Adhere to strict head positioning as instructed by the surgeon.
- Avoid air travel and significant altitude changes until the gas bubble is fully absorbed.
- Monitor for any signs of increased intraocular pressure or infection and report them promptly.
Results
When performed on suitable candidates, pneumatic retinopexy has a success rate of approximately 75% to 90%. Most patients experience significant improvement in retinal attachment and vision.
Conclusion
Pneumatic retinopexy is an effective and minimally invasive procedure for treating specific retinal detachments. Its success relies on careful patient selection, meticulous surgical technique, and strict adherence to postoperative care. For many patients, it offers a quicker recovery and a less invasive alternative to traditional retinal surgeries.
Author Details:
Dr. Sushruth Appajigowda holds a prominent position as a Cornea, Cataract, Glaucoma, and LASIK Surgeon in Bangalore. He serves as the chief Cataract and Refractive surgeon at Vijaya Nethralaya Eye Hospital, Nagarbhavi Bangalore. Renowned as one of the finest LASIK surgeons nationwide, he brings with him over 12+ years of experience across multiple LASIK platforms, including ZEISS, ALCON, SCHWIND, AMO, and Bausch and Lomb. Having successfully conducted over 5000 LASIK procedures, Dr. Sushruth holds the title of a Certified Refractive Surgeon and a Fellow of the All India Collegium Of Ophthalmology. Furthermore, he stands as a distinguished speaker at various National and International Forums, using his expertise to guide you in selecting the most suitable procedure based on your health requirements.

http://vijayanethralaya.com/link-in-bio/
FAQ
What kind of gas is used in pneumatic retinopexy?
Commonly used gases include sulfur hexafluoride (SF6) and perfluoropropane (C3F8).
What is the difference between pneumatic retinopexy and scleral buckle?
Pneumatic retinopexy is minimally invasive, involving a gas bubble, while scleral buckle requires surgical placement of a band around the eye.
How long does pneumatic retinopexy take?
The procedure typically takes 30-45 minutes.
How much does pneumatic retinopexy cost?
Costs vary depending on location and provider but are generally lower than other retinal surgeries.
What is the success rate of retinopexy?
The success rate ranges from 75% to 90%, depending on the case and adherence to postoperative care.