INTRODUCTION:
The ability to see is something that many of us take for granted until we experience vision loss. For those who have suffered from corneal disease or injury, the darkness that comes with impaired vision can be a frightening and isolating experience. However, with the advancements in cornea transplant surgery, there is now hope for those who once thought they would never see the light again. In this article, we will explore the fascinating world of cornea transplants and how they can restore vision, bringing patients from darkness to light. A cornea transplant, also known as keratoplasty, Cornea transplant surgery is a surgery that involves replacing a damaged or diseased cornea with a healthy one obtained from a donor.
The cornea is the clear outermost layer of the eye that plays a crucial role in focusing light onto the retina, which is responsible for transmitting visual information to the brain. A damaged or diseased cornea can severely impair vision and even cause blindness. A cornea transplant surgery is a safe and effective treatment option for a variety of corneal graft diseases and injuries.

Why it’s done?
Cornea transplants, also known as corneal grafts, are done to restore vision in people who have corneal damage or disease. The cornea is a vital component of the eye, positioned at the front as a clear, dome-shaped surface responsible for focusing the light entering the eye. When the cornea is damaged or diseased, it can cause vision problems such as blurred vision, sensitivity to light, and even blindness. Cornea transplants involve replacing the damaged or diseased cornea with a healthy one from a donor. This surgery can improve vision, relieve pain, and restore the overall health and function of the eye. corneal grafts are typically performed when other treatments, such as medication or contact lenses, have not been successful in improving vision.
Types of cornea transplant procedures:
There are three main types of cornea transplant procedures:
- Penetrating Keratoplasty (PK): This is the traditional cornea transplant surgery, where the entire damaged or diseased cornea is removed and replaced with a healthy donor cornea. The donor cornea is stitched in place using sutures and may take several months to fully heal.
- Descemet’s Stripping Endothelial Keratoplasty (DSEK): This procedure is less invasive than PK and is used to treat corneal endothelial disease. In DSEK, only the innermost layer of the cornea called the endothelium, is replaced with a thin layer of donor tissue. The donor tissue is attached to the back of the patient’s cornea using an air bubble, and the patient’s own cornea is left in place.
- Descemet’s Membrane Endothelial Keratoplasty (DMEK): This is the most advanced form of cornea transplant surgery and is also used to treat corneal transplant surgery endothelial disease. DMEK is similar to DSEK, but instead of a thin layer of donor tissue, only the donor Descemet’s membrane and endothelium are transplanted. This procedure has a faster recovery time and fewer risks compared to the other two types of cornea transplant surgery.
There are two main types of partial-thickness cornea transplant operations:
- Lamellar Keratoplasty: This procedure involves replacing only the damaged or diseased layer of the cornea. There are two types of lamellar keratoplasty, anterior and posterior, which involve removing the front or inner layers of the cornea and replacing them with a donor tissue graft. Both procedures have shorter recovery times than full-thickness cornea transplants.
- Endothelial Keratoplasty: This procedure focuses on the innermost layer of the cornea, called the endothelium.The damaged or diseased endothelium is removed and replaced with a healthy donor graft. There are two types of endothelial keratoplasty, Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) and Descemet’s Membrane Endothelial Keratoplasty (DMEK), both of which have faster recovery times than full-thickness cornea transplants.
Partial-thickness cornea transplant procedures can be a suitable option for patients with certain types of corneal disease or damage. However, the appropriate procedure depends on the individual needs of each patient and should be determined in consultation with an experienced ophthalmologist.
Cornea Transplants causes:
Cornea transplants, like any surgical procedure, can have potential risks and complications. Some of the most common causes and risks associated with cornea transplant surgery include:
- Rejection: The patient’s immune system may recognize the donor cornea as foreign and attack it, causing the transplant to fail. Rejection can occur at any time after surgery and may require additional treatment, such as medication or another transplant.
- Infection: every surgical procedure has the potential to result in an infection.
- . Patients who have cornea transplants are at risk for infections that can occur in the eye and may require treatment with antibiotics or other medications.
- Cataracts: In some cases, patients may develop cataracts after cornea transplant surgery. Cataracts occur when the natural lens of the eye becomes cloudy and can cause vision problems.
- Glaucoma: Patients who have cornea transplants may be at risk for developing glaucoma, a condition that occurs when pressure builds up in the eye and damages the optic nerve.
- Astigmatism: After cornea transplant surgery, patients may experience astigmatism, which is a condition where the cornea is irregularly shaped and causes blurred vision.
Cornea Transplants treatments:
Cornea transplant surgery is the main treatment for corneal damage or disease. However, there are several other treatments that can be used in conjunction with or instead of cornea transplant surgery:
- Medications: Eye drops, ointments, and oral medications can be used to treat certain types of corneal diseases and conditions. For example, antibiotics may be prescribed to treat infections, while corticosteroids can reduce inflammation and promote healing.
- Contact lenses: In some cases, contact lenses can be used to improve vision in patients with corneal damage or disease. Scleral contact lenses, which rest on the white part of the eye rather than the cornea, may be used for patients with severe corneal scarring.
- Amniotic membrane grafts: These are used to treat severe corneal ulcers and other types of corneal damage. A piece of amniotic membrane, which is obtained from the innermost layer of the placenta, is placed over the damaged area of the cornea to promote healing and reduce scarring.
- Corneal cross-linking: This is a non-surgical procedure used to treat keratoconus, a condition where the cornea becomes thin and cone-shaped. During corneal cross-linking, special eye drops are applied to the cornea, which is then activated by ultraviolet light. This strengthens the cornea and can prevent further thinning and distortion.
- Intacs: These are small, plastic inserts that are placed into the cornea to treat keratoconus. Intacs help to reshape the cornea, improve vision, and reduce the need for cornea transplant surgery.
Cornea Transplants prevention:
Corneal damage or disease can sometimes be prevented through certain measures, such as:
- Eye protection: Wearing eye protection, such as safety glasses or goggles, can help prevent corneal injuries from occurring during sports, work, or other activities that may pose a risk.
- Proper contact lens use: Proper hygiene and care of contact lenses can help prevent infections and other complications that may damage the cornea. This includes washing hands before handling lenses, using only sterile solutions, and replacing lenses as recommended.
- Regular eye exams: Regular eye exams can help detect early signs of corneal disease or damage, allowing for prompt treatment and preventing further complications.
- Managing underlying conditions: Certain conditions, such as diabetes and autoimmune diseases, can increase the risk of corneal damage or disease. Managing these conditions through proper medical care and lifestyle modifications can help reduce this risk.
- Avoiding harmful substances: Exposure to certain chemicals or substances, such as cleaning solutions or cigarette smoke, can irritate or damage the cornea. Avoiding these substances or taking appropriate precautions, such as wearing gloves or a mask, can help prevent damage.
While some causes of corneal damage or disease may not be preventable, taking these steps can help reduce the risk of complications and protect the health of the eyes.
How you prepare for a cornea transplant surgery:
Preparing for cornea transplant surgery involves several steps, including:
- Medical Evaluation: Your eye doctor will perform a thorough examination of your eyes and medical history to determine if you are a good candidate for cornea transplant surgery. This may involve a series of tests, such as a visual acuity test, a corneal thickness measurement, and a slit-lamp examination.
- Donor Tissue Matching: Once you are deemed a suitable candidate for cornea transplant surgery, your doctor will determine the best match for a donor cornea. This involves assessing the size and shape of your cornea, as well as the quality and availability of donor tissue.
- Medications: Before the surgery, you may be prescribed medications to help prevent infection and inflammation.
- Fasting: You will likely be instructed to avoid food and drink for several hours prior to the surgery.
- Transportation: You will need to arrange transportation to and from the surgical facility, as you will not be able to drive immediately after the procedure.
It is important to follow your doctor’s instructions carefully in the days leading up to your cornea transplant surgery to ensure the best possible outcome.
Finding a donor cornea:
Finding a donor cornea is an important step in the process of cornea transplant surgery. Here are some important things to know about how donor corneas are obtained:
- Donation: Corneas are typically obtained from deceased donors who have given consent for their organs and tissues to be used for transplantation.
- Screening: Donor corneas undergo a thorough screening process to ensure they are safe and suitable for transplantation. This includes testing for infectious diseases and evaluating the quality of the tissue.
- Matching: The donor cornea is matched to the recipient based on factors such as the size, shape, and curvature of the cornea.
- Waiting list: Individuals requiring cornea transplants are added to a list and must wait until a compatible cornea from a donor is obtainable.
- The length of time a patient may need to wait can vary depending on factors such as the availability of donor tissue and the urgency of the patient’s condition.
- Consent: Patients who receive a cornea transplant must give informed consent for the procedure, which includes understanding the risks and benefits of the surgery and the potential for complications or rejection.
It is important to note that cornea transplantation is only possible through the generosity of donors and their families. Individuals who are interested in becoming organ and tissue donors can register with their local organ donation registry or indicate their wishes on their driver’s license or state ID card.
During the procedure:
During a cornea transplant procedure, you will be given anesthesia to ensure that you are comfortable and pain-free. The procedure itself typically takes one to two hours to complete and involves the following steps:
- Preparation: Your eye will be thoroughly cleaned and sterilized, and your doctor will use a special device to hold your eye open during the procedure.
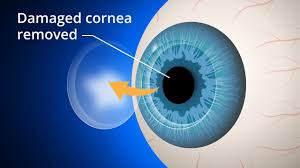
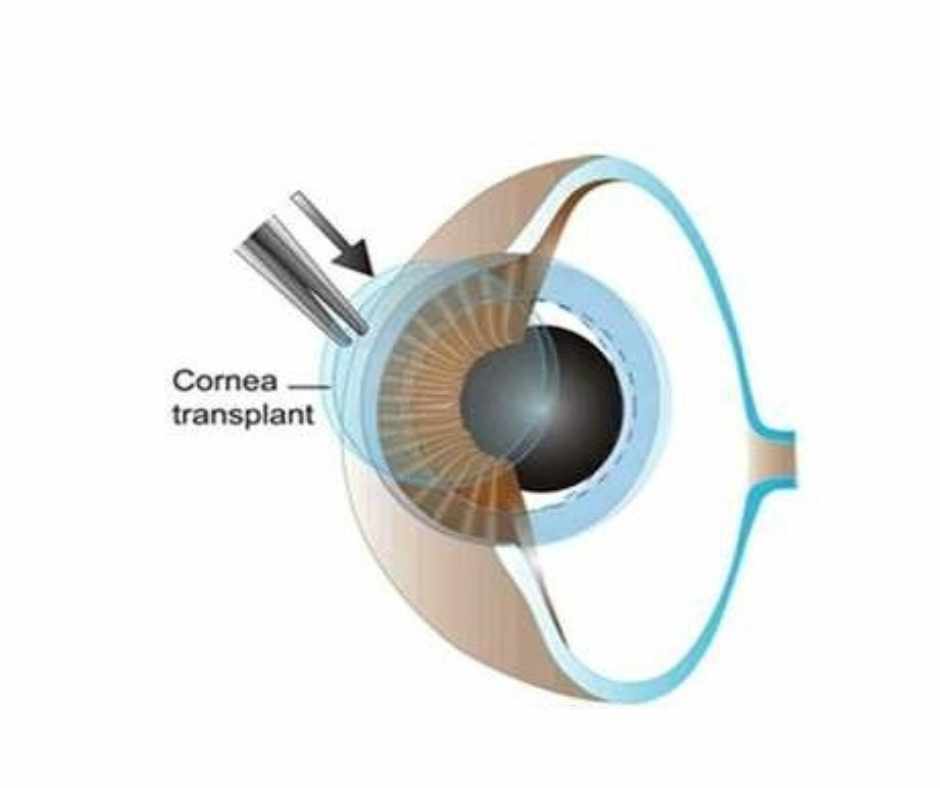
- Incision: Your doctor will make a small incision in the eye to access the damaged or diseased portion of the cornea.
- Donor Tissue: The donor tissue will be carefully prepared and placed onto the eye.
- Sutures: The donor tissue will be secured in place using tiny sutures or other techniques, such as an adhesive.
- Eye Patching: After the procedure is complete, your eye will be covered with a protective eye patch or shield to aid in healing.
After the surgery, you will be monitored for a short period of time to ensure that there are no complications, such as bleeding or infection. Once your doctor is satisfied with your progress, you will be able to return home to begin your recovery.
After the procedure:
After cornea transplant surgery, it is important to follow your doctor’s post-operative instructions carefully to ensure a successful recovery. These may include:
- Eye Patching: You will likely be instructed to wear a protective eye patch or shield for a period of time after the surgery to protect your eye as it heals.
- Medications: You may be prescribed eye drops or other medications to help prevent infection and reduce inflammation. It is important to use these medications as directed by your doctor.
- Follow-up Appointments: You will need to attend several follow-up appointments with your eye doctor in the weeks and months after the surgery to monitor your progress and ensure that the transplant is successful.
- Restrictions: You may be advised to avoid strenuous activities or heavy lifting for a period of time after the surgery to prevent damage to the eye.
- Healing Time: It can take several months for the eye to fully heal and for vision to improve. In some cases, vision may not fully return to normal, and you may require additional treatments or surgeries.
It is important to be patient and follow your doctor’s instructions closely during the recovery process to give your eye the best chance of healing successfully.
RESULTS:
The results of cornea transplant surgery can vary depending on the individual and the specific circumstances of the transplant. In general, however, many patients experience significant improvement in their vision and quality of life following the procedure.
Some potential outcomes of cornea transplant surgery may include:
- Improved Vision: For many patients, cornea transplant surgery results in improved vision, including clearer, sharper, and more detailed vision.
- Reduced Pain: If the cornea was causing discomfort or pain before the surgery, many patients report a significant reduction in these symptoms following the transplant.
- Enhanced Quality of Life: Improved vision and reduced pain can lead to an overall improvement in quality of life, allowing patients to perform daily activities more easily and comfortably.
- Risks and Complications: As with any surgical procedure, there are risks and potential complications associated with cornea transplant surgery. These may include infection, bleeding, rejection of the donor tissue, and other issues.
It is important to discuss the potential outcomes and risks of cornea transplant surgery with your eye doctor prior to the procedure to ensure that you have a clear understanding of what to expect.
Vision correction after surgery:
Cornea transplant surgery can help to correct vision problems caused by a damaged or diseased cornea. After the surgery, it is common for patients to experience some fluctuations in their vision as the eye heals and adjusts to the new tissue.
In some cases,
- Eyeglasses: In many cases, patients can achieve clear vision with the use of eyeglasses following a cornea transplant.
- Contact Lenses: Contact lenses may be an option for some patients to help correct any remaining vision problems after the surgery.
- Laser Eye Surgery: In some cases, laser eye surgery such as LASIK may be recommended to further improve vision after a cornea transplant, and cornea transplant cost is also affordable.
It is important to discuss any concerns about vision correction with your eye doctor both before and after the surgery to ensure that you have a clear understanding of your options and the potential outcomes.
VijayaNethralaya Eye Hospital Bangalore Cornea Transplant Cost:
The Cornea Transplant Cost at VijayaNethralaya: Eye Hospital in Bangalore can vary depending on the type of cornea transplant cost and procedure required and the individual needs of the patient. On average, a cornea transplant price at this hospital ranges from approximately INR 60,000 to INR 100,000. However, it’s important to consult with our expert doctors to determine the exact cost of your cornea transplant price, as it may vary based on your specific requirements and the type of procedure recommended by the doctor. for more information, you can book an appointment and consult with our doctors.
Contact us today
Conclusion:
In conclusion, a cornea transplant is a safe and effective treatment option for a variety of corneal diseases and injuries. The procedure can significantly improve vision and quality of life for patients. It is important for patients to carefully follow their surgeon’s instructions and attend all follow-up appointments to ensure proper healing and monitor for any complications. With proper care, a cornea transplant surgery can be a life-changing procedure for those in need and Cornea Transplant Cost is also budget-friendly.
FAQS:
What is a cornea transplant?
- A cornea transplant is a surgical procedure in which damaged or diseased corneal tissue is replaced with healthy donor tissue to restore vision.
How is the donor tissue obtained?
- Donor tissue for a cornea transplant is typically obtained from a deceased donor through an eye bank.
What conditions can be treated with a cornea transplant?
- Cornea transplant surgery can be used to treat a variety of conditions, including keratoconus, Fuchs’ dystrophy, corneal scarring, and other diseases or injuries that affect the cornea.
Which are the different types of cornea transplant surgery procedures?
- The three main types of cornea transplant procedures are penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK), and endothelial keratoplasty (EK).
What is the duration of the recovery period after a cornea transplant surgery?
- Recovery times can vary depending on the individual and the specific procedure performed, but most patients can expect to need several weeks or months to fully recover from a cornea transplant.
What are the risks and potential complications associated with cornea transplant surgery?
- Like any surgical procedure, cornea transplant surgery carries some risks and potential complications, including infection, rejection of the donor tissue, and other issues.