Introduction:
Glaucoma is a group of eye diseases that damage the optic nerve, which connects the eye to the brain. It is often associated with increased pressure in the eye, known as intraocular pressure (IOP). If left untreated, glaucoma can lead to permanent vision loss and even blindness. Therefore, early diagnosis and appropriate treatment are crucial.
Understanding Glaucoma:
WHAT IS GLAUCOMA AND HOW DOES IT OCCUR?
Glaucoma, a leading cause of preventable blindness, affects approximately 2.2% of the population. Regular eye examinations are crucial to detect the disease early, as it often has no noticeable symptoms. Without proper treatment, glaucoma can lead to permanent and irreversible blindness. The condition is characterized by increased pressure in the eye, which damages the optic nerve. However, with regular consultation and adherence to treatment, the majority of patients can preserve their vision over time.
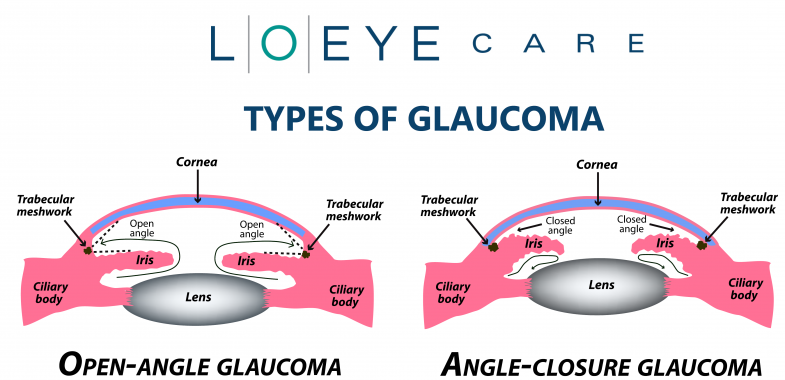
TYPES OF GLAUCOMA:
Open-angle glaucoma: is the most prevalent type and accounts for at least 90% of all glaucoma cases. It is a lifelong condition characterized by the slow passage of fluid through the spongy tissue at the junction of the iris and cornea. Over time, the increased pressure within the eye damages the optic nerve, resulting in vision impairment. Initially, this type of glaucoma is painless and does not cause noticeable changes in vision. However, if left untreated, it can eventually lead to vision loss. Individuals with high blood pressure or diabetes are at a higher risk for developing open-angle glaucoma.
Normal-tension glaucoma: is a subtype of open-angle glaucoma that occurs in individuals with normal eye pressure. Despite the absence of elevated intraocular pressure, optic nerve damage and vision loss still occur.
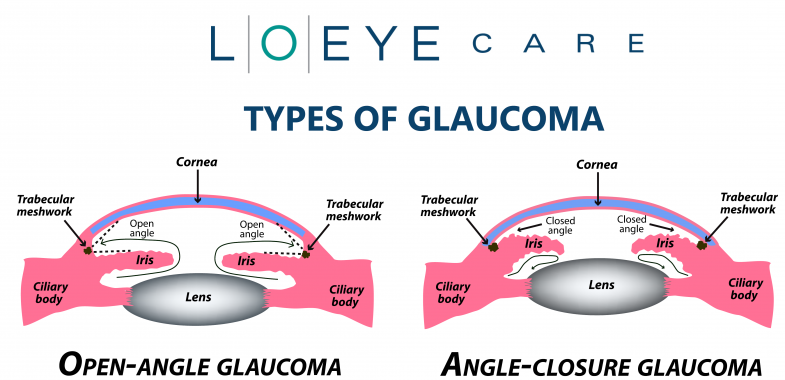
Angle-closure glaucoma: also known as narrow-angle glaucoma, occurs when the drainage passage in the eye becomes narrowed. This can be due to a smaller eyeball size (common in individuals with high positive refractive error) or thickening of the lens caused by cataract development. The outer edge of the iris comes close to the drainage angle in the eye, obstructing fluid drainage. As a result, eye pressure increases rapidly, leading to a sudden and acute rise in intraocular pressure. Without prompt treatment, this type of glaucoma can cause blindness within a few days. It is a painful condition and considered a medical emergency that requires immediate attention from an ophthalmologist. Due to their relatively smaller eye size, individuals of Indian/Asian descent are more frequently observed to have angle-closure glaucoma.
If you experience the following sudden symptoms, it is important to seek immediate medical assistance, as they may indicate angle-closure glaucoma:
- Intense eye pain
- Nausea or upset stomach
- Redness in the eye
- Blurred vision
If you notice any of these symptoms, it is crucial to visit your doctor or go to the nearest emergency room without delay.
Secondary glaucoma refers to glaucoma that occurs as a result of other pre-existing medical conditions, including diabetes, hypertension, eye trauma, inflammation or infection, certain medications such as topiramate or steroids, the presence of cataracts, and intraocular tumors.
Congenital glaucoma is a rare condition in which infants are born with an eye abnormality that disrupts the normal drainage of fluid. It affects only about 1 in every 10,000 babies born. Children with congenital glaucoma often exhibit symptoms such as cloudy eyes, sensitivity to light, excessive tearing, and the possibility of having larger-than-normal eyes. Fortunately, surgery has proven to be highly effective in treating congenital glaucoma.
In addition to congenital glaucoma, there are several other types of glaucoma that can develop in children. Medical professionals generally refer to any form of glaucoma that affects babies or children as pediatric glaucoma.
It is crucial to promptly identify and manage glaucoma in children to prevent vision loss and support healthy eye development.
Consult Now
High-Risk Groups for Glaucoma:
Glaucoma is a condition that can affect people of various age groups, including children, teenagers, and both younger and older adults. Certain factors increase the risk of developing glaucoma. These include:
- Age: The incidence of glaucoma tends to rise with age, making individuals over 60 years old more susceptible.
- Family History: Having a family history of glaucoma increases the likelihood of developing the condition.
- Refractive Errors: Individuals who are highly nearsighted (myopic) or farsighted (hyperopic) have a higher risk of glaucoma.
- Steroid Medications: Prolonged use of steroid medications can contribute to the development of glaucoma.
- Central Cornea Thickness and Intraocular Pressure: Having a thin central cornea or elevated intraocular pressure can be risk factors for glaucoma.
- Eye injuries, sleep apnea, and migraines have also been linked to an increased risk of glaucoma.
Understanding Glaucoma: Silent Progression and Recognizing Symptoms
Glaucoma: A Silent Disease with Gradual Progression:
Glaucoma is a stealthy disease that often develops without noticeable symptoms for an extended period of time. Doctors frequently detect glaucoma during routine general examinations.Early detection plays a pivotal role in safeguarding your vision from the detrimental effects of glaucoma. Progression of the disease may eventually lead to the manifestation of certain symptoms in some patients, including:
- Unusual difficulty adjusting to dark environments.
- Challenges in focusing on objects, whether they are nearby or at a distance.
- Recurrent pain in or around the eyes.
- Perception of rainbow-colored “halos” or colored rings around light sources.
- Excessive tearing or watering of the eyes.
- Nausea or vomiting accompanied by severe eye pain.
- In advanced stages, the loss of peripheral vision, commonly referred to as tunnel vision.
Diagnosing and Monitoring Glaucoma:
- Tonometry: Measuring Eye Pressure Tonometry is a method used to measure the pressure inside the eye using a tonometer. This test is essential for evaluating the effectiveness of glaucoma treatment and monitoring disease progression. The normal range for eye pressure is typically between 10-21mmHg. However, it’s important to consider that corneal thickness can influence the readings. Thicker corneas may result in higher pressure readings, while thinner corneas may lead to lower readings. To obtain accurate pressure measurements, a corneal thickness measurement, known as pachymetry, is necessary.
- Gonioscopy: Assessing the Eye’s Drainage Angle Gonioscopy is an eye examination that focuses on detecting signs of glaucoma. It involves using a special lens and slit lamp to evaluate the drainage angle, also known as the anterior chamber angle, in the eye. This test helps differentiate between open-angle and closed-angle glaucoma, guiding treatment decisions accordingly.
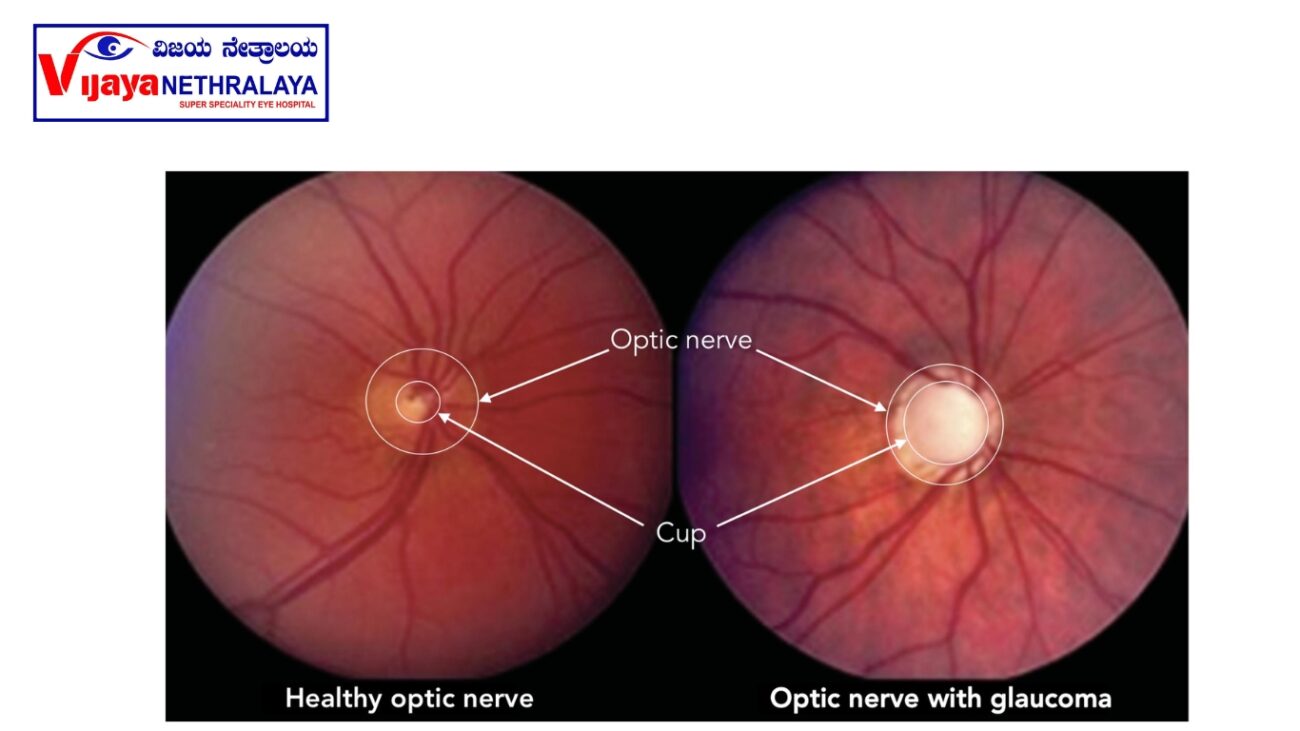
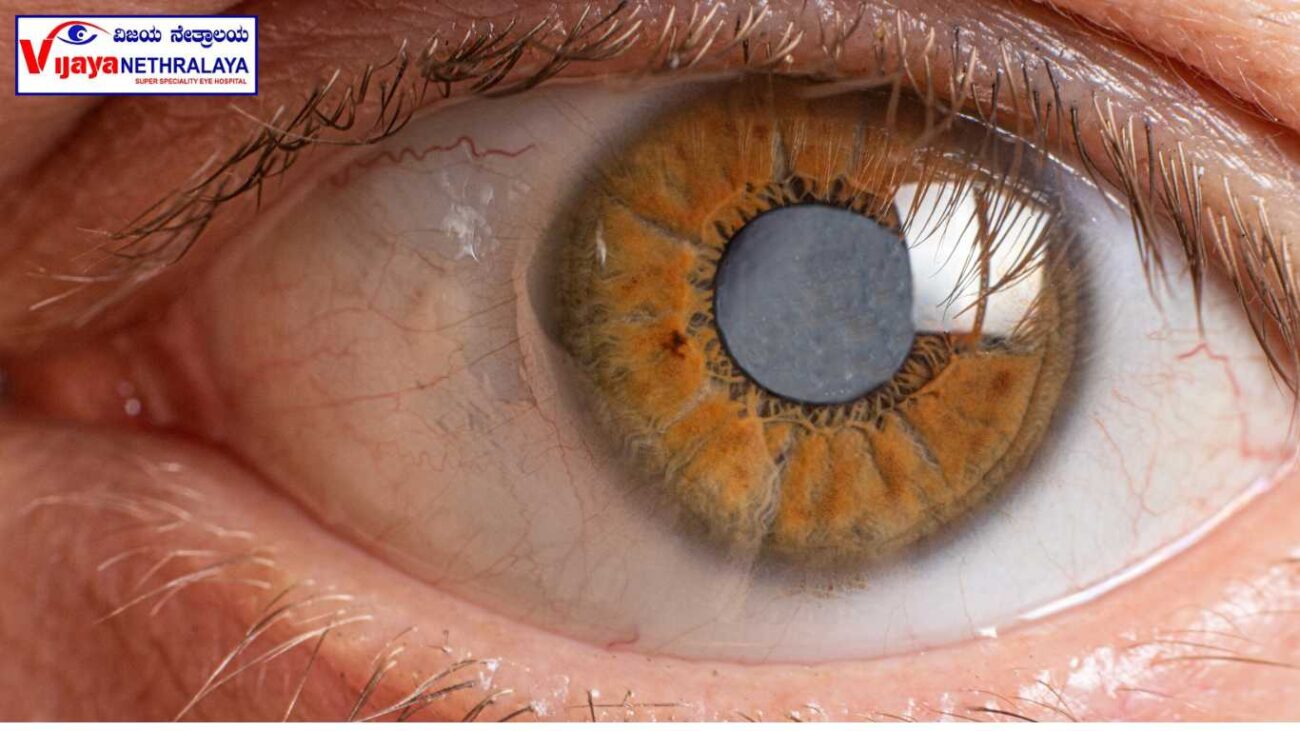
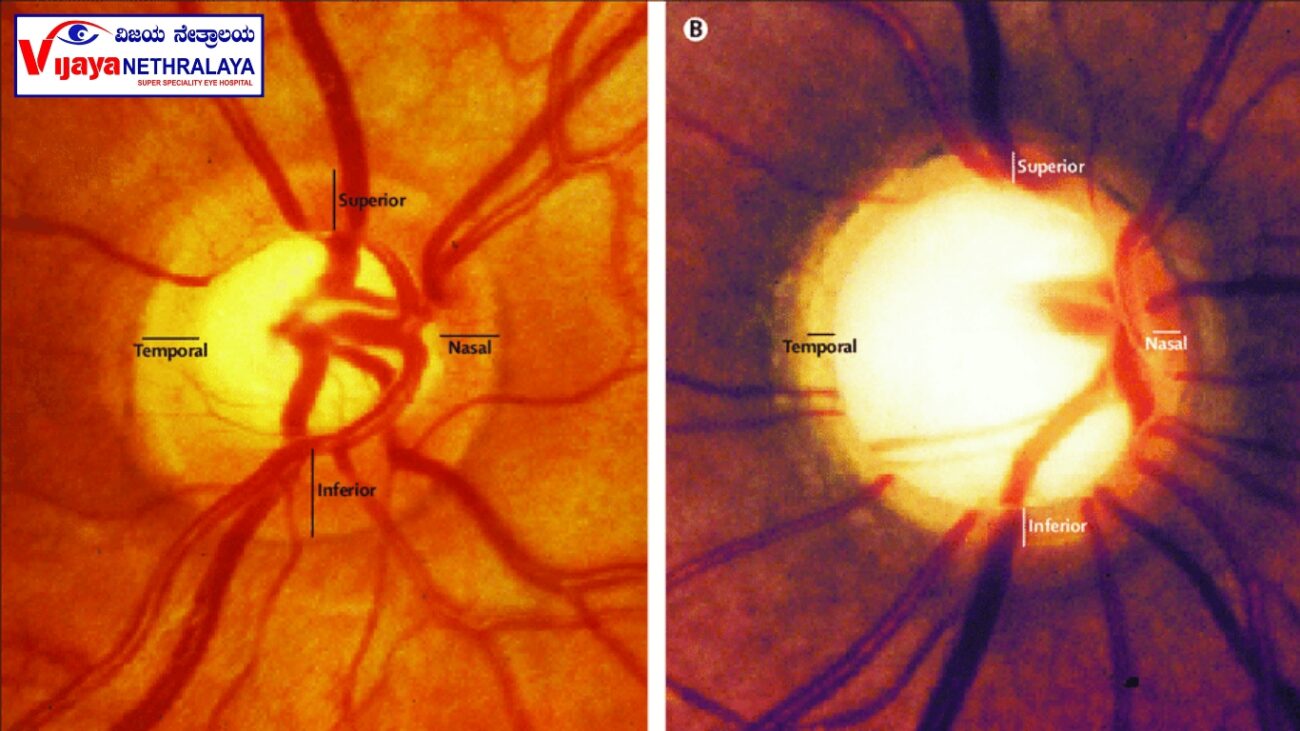
- Dilated Eye Exam: Assessing Retinal Health During a dilated eye exam, eye drops are administered to widen or dilate the pupils. This allows the eye care professional to examine the retina and optic nerve for signs of damage and other eye conditions. The effects of the drops usually last for a few hours, during which close-up vision may remain blurred.
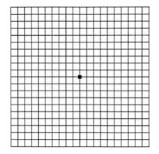
- Visual Field Test: Assessing Peripheral Vision A visual field test is a computerized assessment of the peripheral vision. It can detect any loss of vision in the outer areas of the visual field, which is indicative of glaucoma. During the test, the patient sits in front of a concave bowl-like machine and focuses on a central target. The machine then flashes small spots of light with varying intensities, and the patient must press a button when they perceive the lights. This test helps track visual field defects and monitor disease progression”For individuals with established glaucoma, doctors typically conduct this test at least once a year and may perform it more frequently based on the severity and progression of the disease.”
- Optical Coherence Tomography (OCT): Evaluating Optic Nerve Health OCT is an advanced and highly accurate test used to assess the optic nerve and detect any structural damage. This non-invasive imaging technique employs a low-powered laser to create detailed 3D, color-coded cross-sectional images of the layers of the retina and optic nerve. OCT is particularly useful in the early stages of glaucoma, providing valuable information for determining treatment protocols and monitoring disease progression.
- Pachymetry: Measuring Corneal Thickness Pachymetry involves measuring the thickness of the cornea, the black part of the eye. This measurement plays a crucial role in obtaining accurate eye pressure readings. The eye care professional applies a numbing drop to the eye and employs an ultrasonic wave instrument to measure the corneal thickness.
Glaucoma Treatment:
- Medications: Eye drops or oral medications are often prescribed to reduce IOP. These medications either decrease fluid production in the eye or improve its drainage. It is important to use the prescribed medications as directed by the ophthalmologist and to regularly follow up for monitoring.
- Laser Therapy: Laser treatment can be used to improve the drainage of fluid in the eye or reduce its production. Types of laser treatment for glaucoma include:
- Selective Laser Trabeculoplasty (SLT): This laser treatment helps improve the drainage of fluid from the eye by targeting the trabecular meshwork.
- In laser peripheral iridotomy (LPI), doctors perform a procedure to create a small hole in the iris for angle-closure glaucoma, enabling better fluid flow. Cyclophotocoagulation: This laser treatment targets the ciliary body to reduce fluid production in cases where other treatments are ineffective.
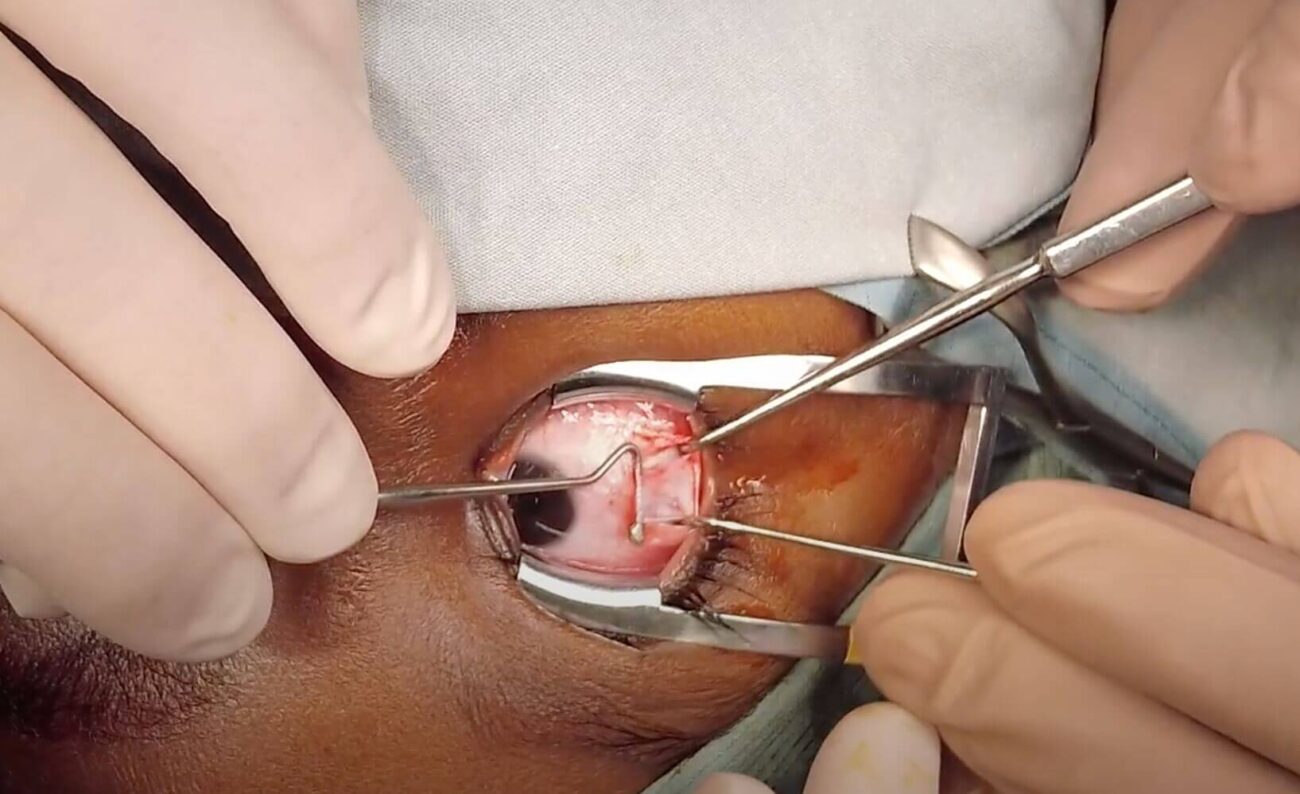
- In cases where medication and laser therapy do not effectively control glaucoma or the disease is advanced, doctors may deem surgery necessary.
- Different surgical procedures are available, including:
- Lifestyle Changes: Certain lifestyle modifications can help manage glaucoma and reduce the risk of progression. These include avoiding excessive eye strain, practicing regular exercise, maintaining a healthy diet, and managing other systemic conditions such as diabetes and hypertension.
Author Details:
Dr. Ravina Todi is a skilled Ophthalmologist specializing in glaucoma. With an MS in Ophthalmology, she has extensive experience in eye treatments and surgeries. Dr. Todi is dedicated to patient care and advancing the field through research and publications. Her expertise in glaucoma management makes her highly regarded in her profession.

Conclusion:
In conclusion, glaucoma is a serious eye disease that can lead to vision loss and blindness if left untreated Glaucoma earns the moniker “silent thief of sight” because it gradually and asymptomatically robs individuals of their vision in the early stages. Nevertheless, through early detection and appropriate treatment, healthcare professionals can effectively manage the progression of glaucoma and preserve patients’ vision.