Understanding Choroidal Neovascular Membrane: Causes, Diagnosis, and Treatment
INTRODUCTION:
Choroidal Neovascular membrane (CNVM) is a leading cause of central vision loss. It involves the growth of abnormal and leaky blood vessels under the retina (the light-sensitive part of the eye) and is seen mostly in the macula region which is the central part of the retina. These blood vessels grow from the capillaries of the underlying choroid (the vascular layer which also supplies blood supply to the retina) and are extremely fragile and prone to bleeding. It is mainly seen in the elderly population when associated with macular degeneration but can be seen in other age groups as well based on the etiology.
Causes Of Choroidal Neovascular Membrane:
- WET Age-related macular degeneration (ARMD): It is the most common cause of CNVM formation. Wet ARMD constitutes 10-15% of ARMD and is characterized by the presence of CNVM.
- High Myopia-High minus power is a risk factor for CNVM formation due to axial elongation. The incidence of CNVM in pathological myopia is approximately 5%.
- Anguloid streaks -this condition of the retina can also lead to CNVM formation. It has been associated with several systemic diseases, including pseudoxanthoma elasticum, Paget's disease of bone, Ehlers-Danlos syndrome, sickle cell disease, thalassemia, and other blood dyscrasias.
- Inflammatory disorders-CNVM in the macular area is a major cause of visual loss in presumed ocular histoplasmosis syndrome (POHS), inflammatory disorders like congenital toxoplasmosis, choroiditis, etc. Usually, CNVM occurs at the edge of an old healed chorioretinal scar.
- Trauma-Traumatic ruptures of the Bruch's membrane called choroidal ruptures in the retina are commonly seen following blunt injuries to the eye. This condition can also cause the development of CNVM. They are usually seen a few weeks or months following the trauma.
- Idiopathic- When CNVM develops in the absence of any pathologies in the eye, it’s called idiopathic.

Painless loss of central vision-Patients complains of blurry vision making it difficult to read and write, sew, and do near work.

Metamorphopsia (perception of distorted images and straight lines appearing curvy) -this reduces the quality of vision, making it difficult to recognize faces and objects.

Central black spot (scotoma) is noted in the advanced stages. Peripheral vision is usually preserved in the majority of cases.
INVESTIGATIONS:
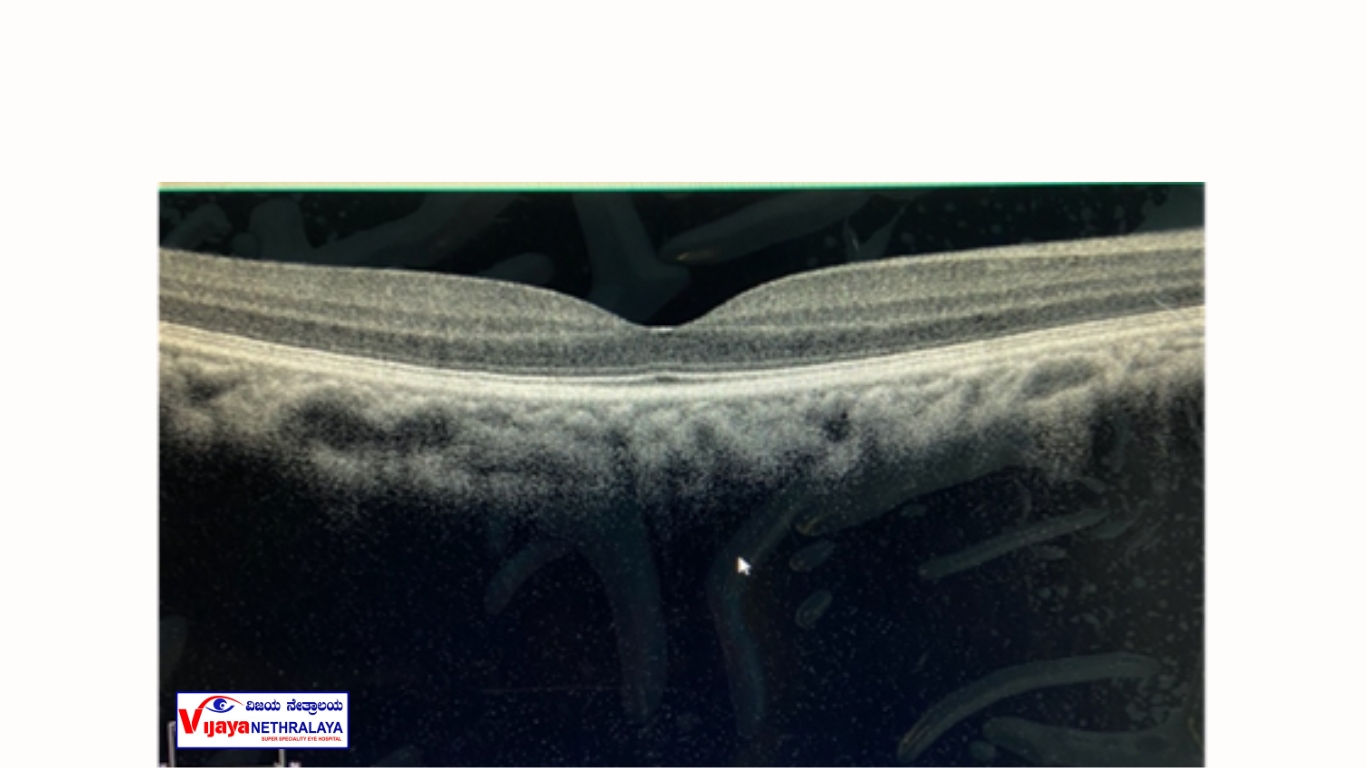
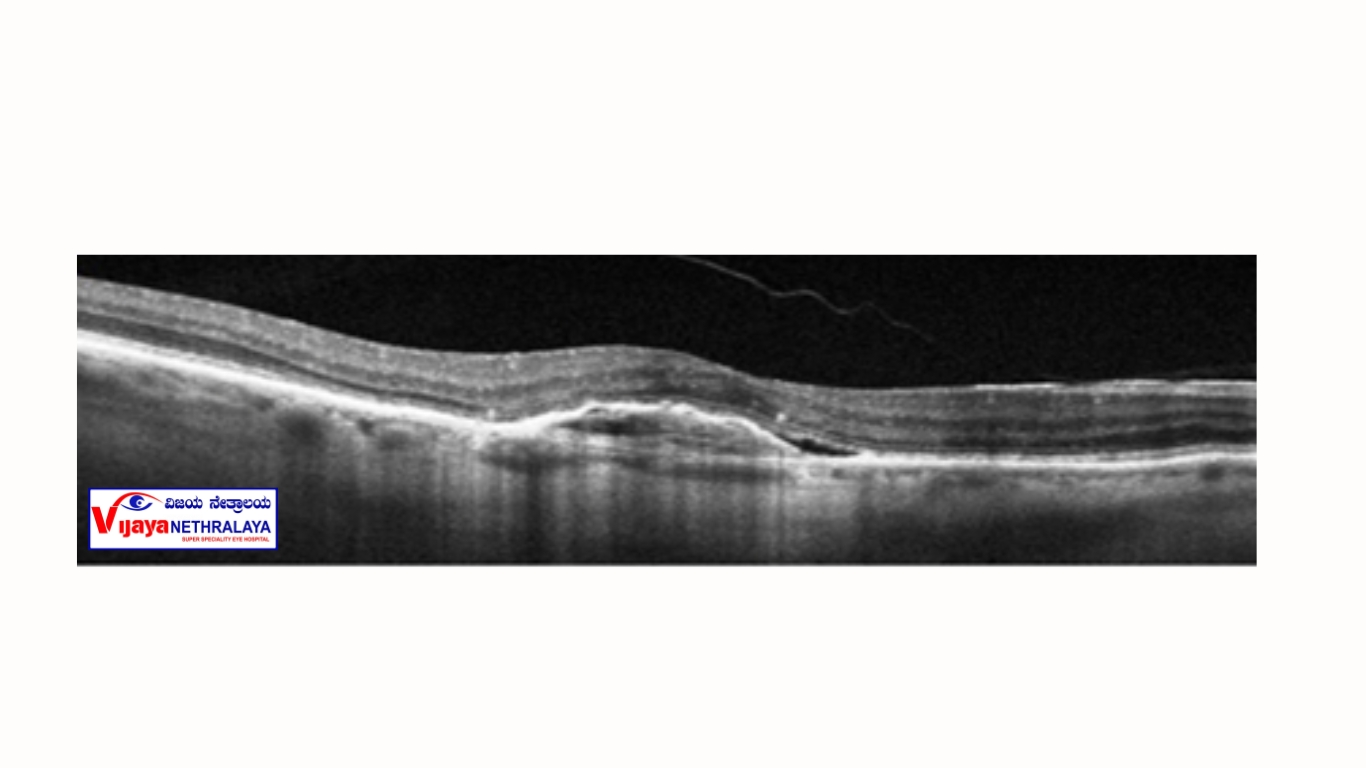
Optical Coherence Tomography (OCT) is the primary diagnostic method used to examine the retina. This quick and noninvasive test provides detailed cross-sectional images of the macula, the central part of the retina where Choroidal Neovascular Membranes (CNVMs) are commonly found. During the OCT scan, your pupils will be dilated, and you will be comfortably seated in front of the OCT machine. You will rest your chin on a chinrest while the scans are taken.

In some cases, the doctor advises a fundus fluorescein angiography (FFA) or Indocyanine green angiography (ICG). The angiography tests involve injecting a dye through the veins and imaging the retina as it runs through the eye circulation.
PROCEDURE for FFA:
After dilating the pupils, an IV line is secured in the patient's forearm. Later an injection of 2-5 ml of sodium fluorescein is administered through the IV line and a series of retinal photographs are taken approximately once every few seconds initially. Delayed images are obtained at 5 and 10 minutes. Rarely, patients may feel nausea during the procedure which is self-limiting. Patients may also observe orange-coloured urine for 24-48 hours post-procedure which is normal.
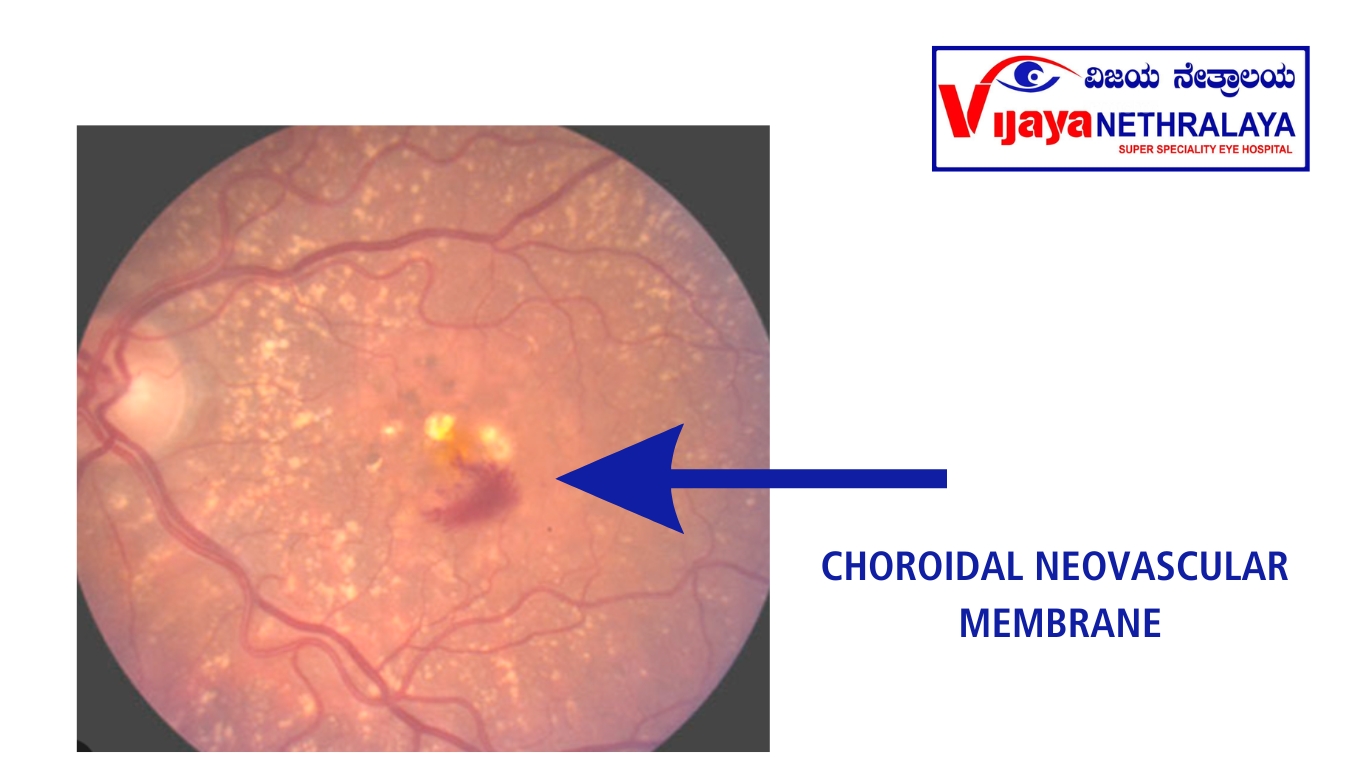
FUNDUS PHOTOS:
Fundus photos are taken using a retinal camera to document the lesion and used to compare during follow-ups.
Intravitreal Injection animation for patient education
The procedure is simple and involves injecting the drug inside the vitreous cavity of the eye. The injections are given under aseptic precautions and topical anesthesia in the operation theatre, through the white part or sclera of the eye using a fine needle by a retina specialist. It is more or less painless and takes about 10 minutes for the procedure. After the injection, the patient is observed for half an hour and is discharged soon after. The patient is advised to use eyedrops for a week and is reviewed by the retina doctor on the next day.
Treatment Of Choroidal Neovascular Membrane:
The mainstay of treatment for CNVM is intravitreal injection of antiangiogenic agents. These include drugs like Bevacizumab, Ranibizumab, Aflibercept, and Brolucizumab. They act by limiting the growth of pathologic blood vessels and controlling disease activity. These injections are given as monthly and bimonthly doses depending on the molecule and disease severity and require a regular follow-up as advised by the treating doctor.
Prevention of Choroidal Neovascular Membrane:
Unfortunately, the onset of this disease cannot be prevented as it is associated with conditions of the eyes people are born with and is hereditary like high myopia, or with natural processes of aging as in AMD. Also, there is a higher risk of development of CNVM in the other eye of affected patients.
Untreated CNVM is an important cause of preventable central visual loss. According to the AREDS -2 study, intake of specific antioxidant tablets in certain cases can help prevent the progression of AMD from the dry to the wet stage. Hence, a regular 6-monthly retina check-up and “self-monitoring at home” for those with risk factors of CNVM are advised. Self-monitoring can be done easily using an Amsler grid chart or as advised by the retina specialist.
Our Retina Specialist Surgeons:
Dr. Pavan K P
MBBS, MS – Ophthalmology

Dr. Sherina Thomas
Medical retina specialist and Vitreo Retinal surgeon, MRCS Edin, FVRS.
Conclusion:
In conclusion, understanding the causes, diagnosing accurately, and providing appropriate treatment for choroidal neovascular membrane are critical in preserving and improving visual function. Advances in medical interventions, particularly anti-VEGF therapy, have significantly improved the prognosis for patients with CNVM, emphasizing the importance of early intervention and ongoing management in the field of ocular care..
