Introduction:
Traumatic glaucoma is a condition that arises as a result of blunt trauma to the eye. Diagnosing and treating traumatic glaucoma promptly is crucial to mitigate its long-term consequences. This introduction provides an overview of traumatic glaucoma, including its causes, symptoms, and potential complications, setting the stage for a deeper exploration of its diagnosis and treatment options. By understanding the importance of early intervention, we can strive to preserve vision and improve the outcomes for individuals affected by traumatic glaucoma.
WHAT IS TRAUMATIC GLAUCOMA?
Ocular injuries are frequently observed in young adults and are a significant contributor to preventable visual impairment. It is crucial to recognize that even minor injuries to or around the eye, which do not necessitate hospital admission, can occasionally have serious and potentially life-threatening consequences. Some of these ocular injuries can later manifest as a secondary cause of glaucoma called traumatic glaucoma. it is important, to make sure to get a regular follow-up eye examination. Traumatic glaucoma is defined clinically as elevation of intraocular pressure(IOP) i.e. eye pressure more than 21mmHg, post-trauma. ( normal IOP 10-21 mmHg). Incidence of development of secondary Glaucoma after blunt injury to the eye is 3.4% at 6 months follow-up and 10% at 10 years follow-up.
All types of ocular injuries have the potential to cause an elevation of the eye pressure in the affected eye through various mechanisms. Without appropriate treatment, this can lead to irreversible glaucomatous damage to the optic nerve and potentially permanent loss of visual function. It can occur by any kind of injury, either that “bruise” the eye ( called blunt trauma), or injuries that penetrate the eye. Conditions like: severe myopia or hypermetropia, previous trauma, infection, or prior surgery in the eye can also make the eye more vulnerable to serious eye trauma. It is most commonly seen in blunt injuries caused by sport-related injuries eg: shuttle cock injury, baseball, and boxing, and are particularly common among the younger age groups. The mainstay of glaucoma treatment is to reduce the eye pressure i.e. the IOP, since elevated IOP remains the main risk factor for glaucomatous optic neuropathy. Surgical interventions are needed when the disease is uncontrolled by medical therapy.
Recognizing the Symptoms of Traumatic Glaucoma:
- Light sensitivity
- Blurred vision
- Aching pain in the eye- can occur immediately after injury
- Blood collection ( hyphema) or inflammation in the eye
- Elevated eye pressure- due to blockage of eye canals with blood and inflammatory cells.
- Some individuals can have increased eye pressure without any of the above symptoms or pain, and an underlying significant optic nerve damage. the patient may remain asymptomatic for a long time until the vision loss has progressed to an advanced stage.
Traumatic Glaucoma secondary to Blunt trauma:
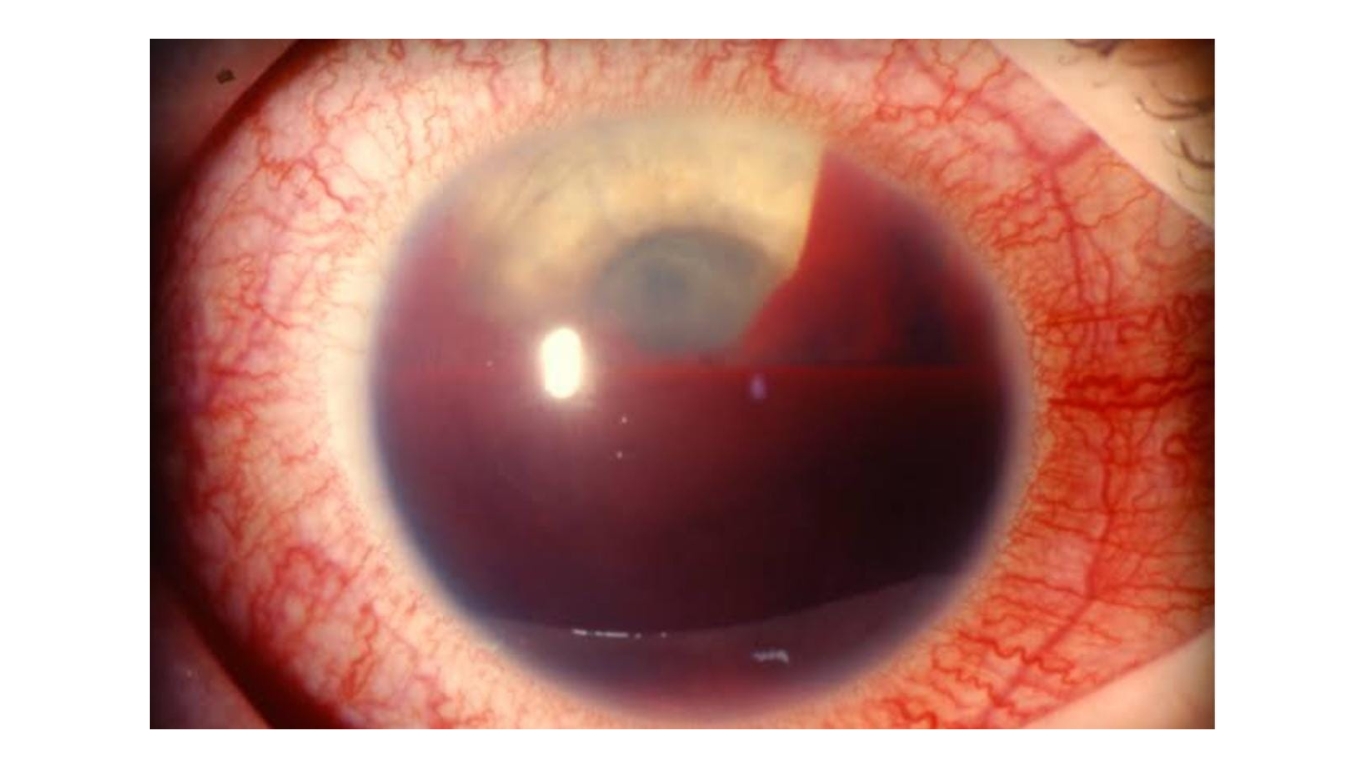
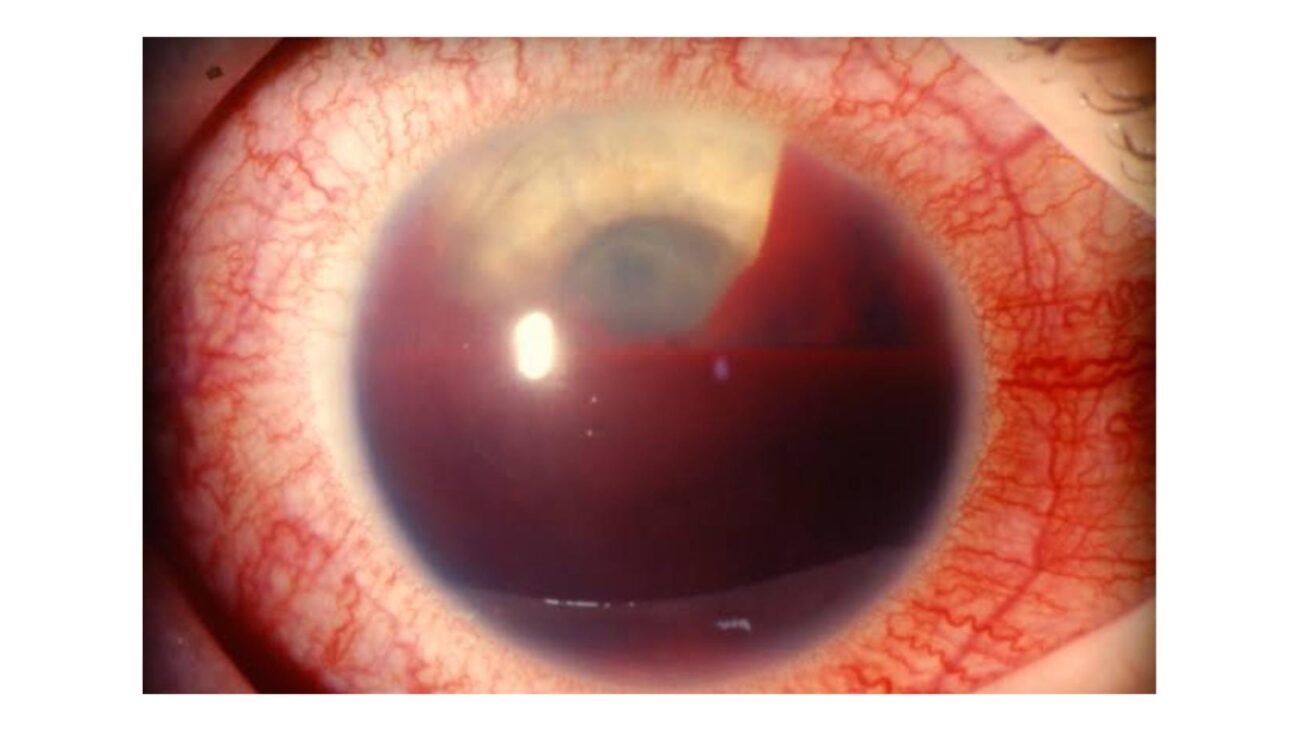
Traumatic Hyphema:
Due to sudden compression-decompression forces in the globe blunt injury to the eye can cause damage to the fragile vascular blood vessels of the ciliary body and stromal iris, leading to bleeding.
Blood accumulation in the anterior chamber can actively obstruct the outflow of aqueous humor through the trabecular meshwork, resulting in an increase in intraocular pressure (IOP). When the entire volume of the anterior chamber is filled with blood, it is referred to as a total hyphema or an “8-ball” hyphema.
The more severe the hyphema, the more severe the complication and risk. Rebleeds can usually occur within 2 to 5 days after the initial bleed and have an incidence of 20-25%, associated with a higher risk of an increase in eye pressure and poor visual outcomes. The goal of the management of traumatic hyphema is to control the eye pressure and prevent re-bleeding. Surgical management is necessary if medical therapy fails to control the intraocular pressure (IOP) or if there is a persistent hyphema lasting more than 5-7 days. Additionally, surgical intervention is indicated in cases of active rebleeding in the eyes.
Traumatic Iritis and Trabecular Meshwork Injury:
Injury to the eye can cause damage to the iris and trabecular meshwork tissue, which can cause increase in vascular permeability and an influx of inflammatory mediators. Inflammatory cells and the precipitates within the AC can block the TM, reducing the aqueous outflow, leading to secondary increase in IOP.
Angle injury:
Depending on the extent of the blunt trauma, there can be damage to the various angle structures. Commonly there is damage to the iris insertion manifesting as angle recession, followed by cyclodialysis and, very uncommonly, iridodialysis. these can be difficult to treat.
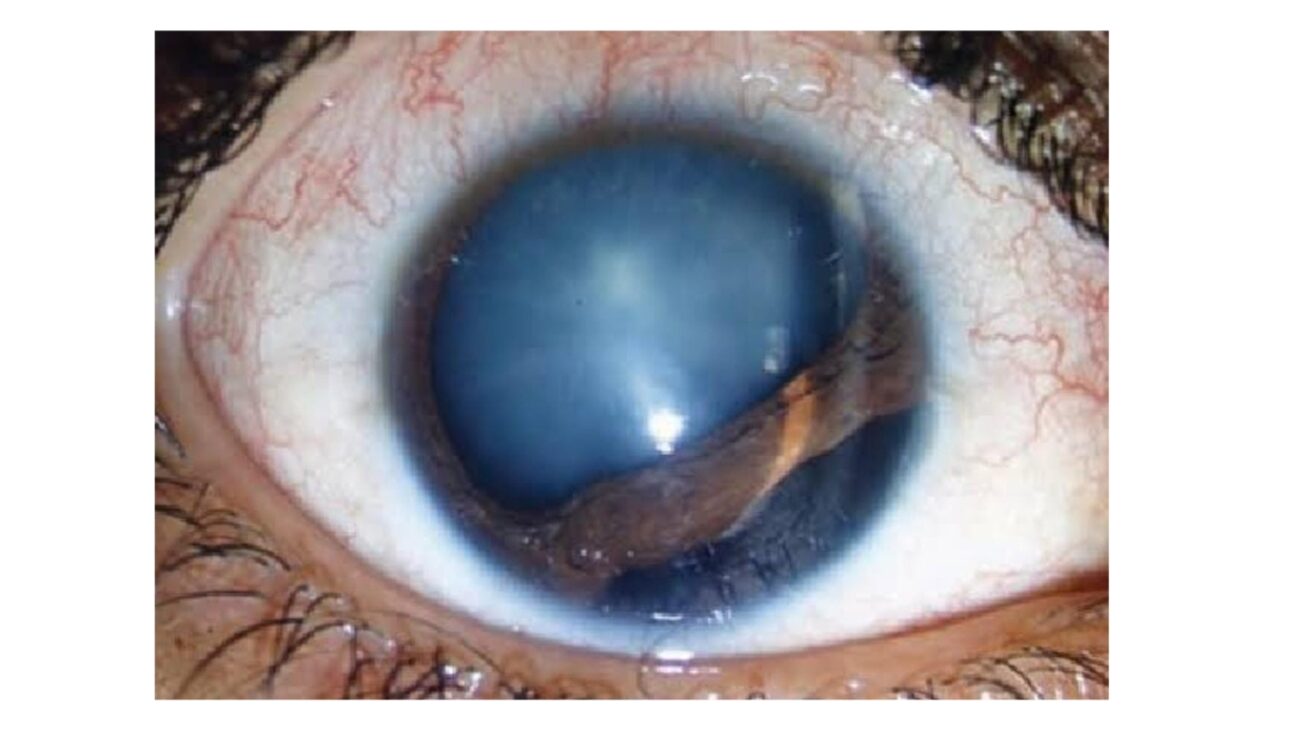
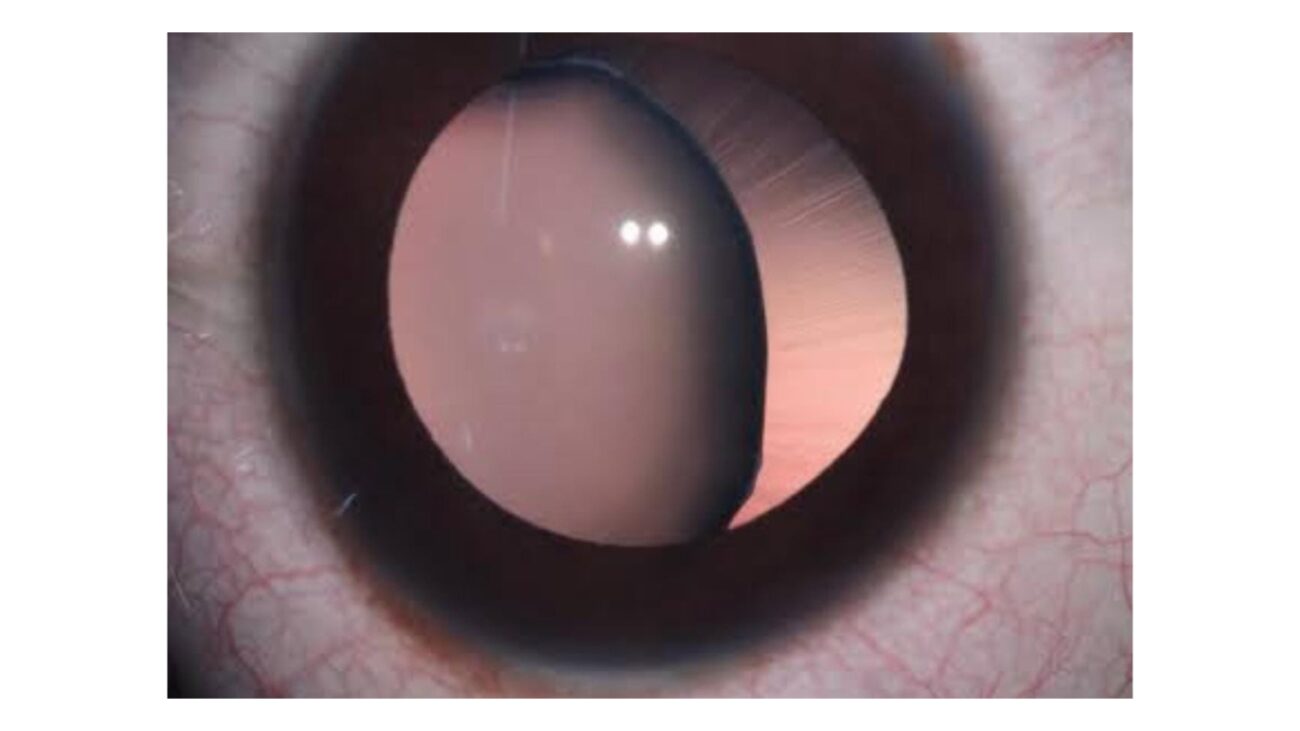
Lens Subluxation and Dislocation with/ without Secondary Pupil Block:
A blunt injury to the eye can actively cause posterior displacement of the lens iris diaphragm, resulting in the rupture of the zonular fibers responsible for holding the lens in position. When more than 25% of the zonules are torn, the lens can be partially displaced from its normal position. Complete dislocation occurs when there is a complete disruption of the zonular fibers.
- when the lens is subluxated anteriorly- it can cause acute angle closure leading to pupillary block and raised IOP.
- Pigments released from chaffing of a displaced lens on the iris can block TM and reduce aqueous outflow and secondary IOP elevation
- In the setting of displaced lens into the vitreous cavity , the vitreous strand can prolapse into the anterior chamber and block the TM, reducing the aqueous outflow and secondary IOP elevation.
Late-onset Steroid Response:
Topical corticosteroid eye drops are commonly used in an ocular trauma setting to reduce intraocular inflammation. Most of the patients develop an associated IOP elevation, commonly 3 to 6 weeks after starting of topical corticosteroid treatment. Therefore, it is utmost important to get your eye pressure checked at every follow-up visit.
Penetrating eye injury:
Traumatic glaucoma can also occur in penetrating injuries caused by sharp instruments. The eye pressure is usually on the lower side initially. But once the wound is closed the eye pressure can rise gradually as the tissue inside the wound becomes swollen and irritated or due to bleeding inside the eye. Eye pressure is initially controlled with medications that reduce the production of eye fluid or those that increase the drainage of the fluid outside the eye. If uncontrolled medically, can go ahead with glaucoma surgeries.
Unmasking the Silent Threat: Diagnosing Traumatic Glaucoma:
- Comprehensive eye examination to know the extent of damage
- Examining the IOP, angle structure and lens status and detailed fundus evaluation (angle structure are measured using gonioscopy lens on slit lamp and IOP by tonometer )
- If sign of optic nerve damage is noticed, following additional tests should be done:
i. optic nerve thickness measurement
ii. visual field test
Restoring Sight: Treatment Approaches for Traumatic Glaucoma:
-The management of traumatic glaucoma focuses on actively lowering the intraocular pressure (IOP) to a normal level, specifically below 21mmHg, while actively preventing further damage to the optic nerve.
-The initial approach focuses on medically reducing the IOP. First-line treatment involves the use of topical therapies such as alpha agonists, beta blockers, carbonic anhydrase inhibitors, or combinations of these drugs.
-In cases where topical medications fail to control IOP, doctors employ oral therapy with acetazolamide tablets or administer mannitol intravenously.
-When maximally tolerated medical therapy proves ineffective in controlling the pressure, doctors consider surgical intervention. They may recommend glaucoma filtering surgery, such as trabeculectomy or placement of a glaucoma drainage device.
-It is crucial to emphasize that if left untreated, traumatic glaucoma can lead to irreversible and permanent damage to the eye and vision. Therefore, it is imperative to undergo a comprehensive eye examination following any injury in or around the eye.
Author details:
Dr. Ravina Todi is a skilled Ophthalmologist specializing in glaucoma. With an MS in Ophthalmology, she has extensive experience in eye treatments and surgeries. Dr. Todi is dedicated to patient care and advancing the field through research and publications. Her expertise in glaucoma management makes her highly regarded in her profession.

Conclusion:
In conclusion, traumatic glaucoma is a serious condition resulting from blunt trauma that can lead to irreversible damage to the eye and vision if left untreated. The primary objective of treatment is to reduce the intraocular pressure (IOP) to a normal level, below 21mmHg, while preventing further harm to the optic nerve. Initial management involves the use of topical medications, such as alpha agonists, beta blockers, and carbonic anhydrase inhibitors. In acute cases, oral therapy or intravenous administration may be necessary. If medical treatment fails to control the IOP adequately, surgical options like glaucoma filtering surgery or drainage devices are considered. It is crucial to emphasize the importance of a comprehensive eye examination following any injury to promptly detect and address traumatic glaucoma.